Overdose Prevention: How to Stay Safe with Medications and Supplements
When we talk about overdose prevention, the set of actions and awareness practices designed to stop accidental or intentional drug overdoses before they happen. Also known as drug safety planning, it’s not just for people using street drugs—it matters just as much if you’re taking prescriptions, over-the-counter painkillers, or even supplements. Too many people think overdoses only happen to others, but the truth is, they often start with a simple mistake: taking one extra pill, mixing meds without knowing the risks, or not realizing how alcohol changes the game.
Medication safety, the practice of using drugs correctly to avoid harm. Also known as drug management, it’s the backbone of overdose prevention. Think about it: if you’re on multiple meds, like a painkiller, an antidepressant, and a sleep aid, you’re already in a high-risk zone. Studies show that over half of opioid overdoses happen to people who were prescribed those drugs legally. It’s not about being careless—it’s about not knowing how things interact. For example, mixing benzodiazepines with opioids can slow your breathing to a dangerous level, even at normal doses. And it’s not just opioids. Acetaminophen, found in dozens of cold and pain meds, can cause liver failure if you take more than 4,000 mg in a day—something many don’t realize because it’s in so many products.
Naloxone, a life-saving medication that reverses opioid overdoses. Also known as Narcan, it’s not just for paramedics anymore. Many pharmacies now sell it without a prescription. Keep it in your home if someone you live with takes opioids, even if it’s for chronic pain. It’s safe, easy to use, and can buy critical minutes until help arrives. And don’t wait for someone to pass out—signs like slow or shallow breathing, blue lips, or unresponsiveness mean act now. You can’t harm someone by giving naloxone if they didn’t take opioids.
Drug interactions are another silent killer. You might not think a common NSAID like ibuprofen could be risky with your blood pressure med, but it can. Or mixing St. John’s Wort with antidepressants? That’s a recipe for serotonin syndrome. The posts below show real cases where people didn’t know what they were mixing—and how simple steps like keeping a meds list or talking to a pharmacist could’ve changed everything.
Overdose prevention isn’t about fear. It’s about knowing your meds, knowing your risks, and having a plan. Whether you’re managing chronic pain, helping an aging parent, or just trying to avoid a bad reaction, the tools are simple: track what you take, ask your doctor or pharmacist about interactions, keep naloxone handy if opioids are involved, and never assume something is "safe" just because it’s sold over the counter. The posts here give you the real, no-fluff details on how to spot danger before it hits—and what to do when it does.
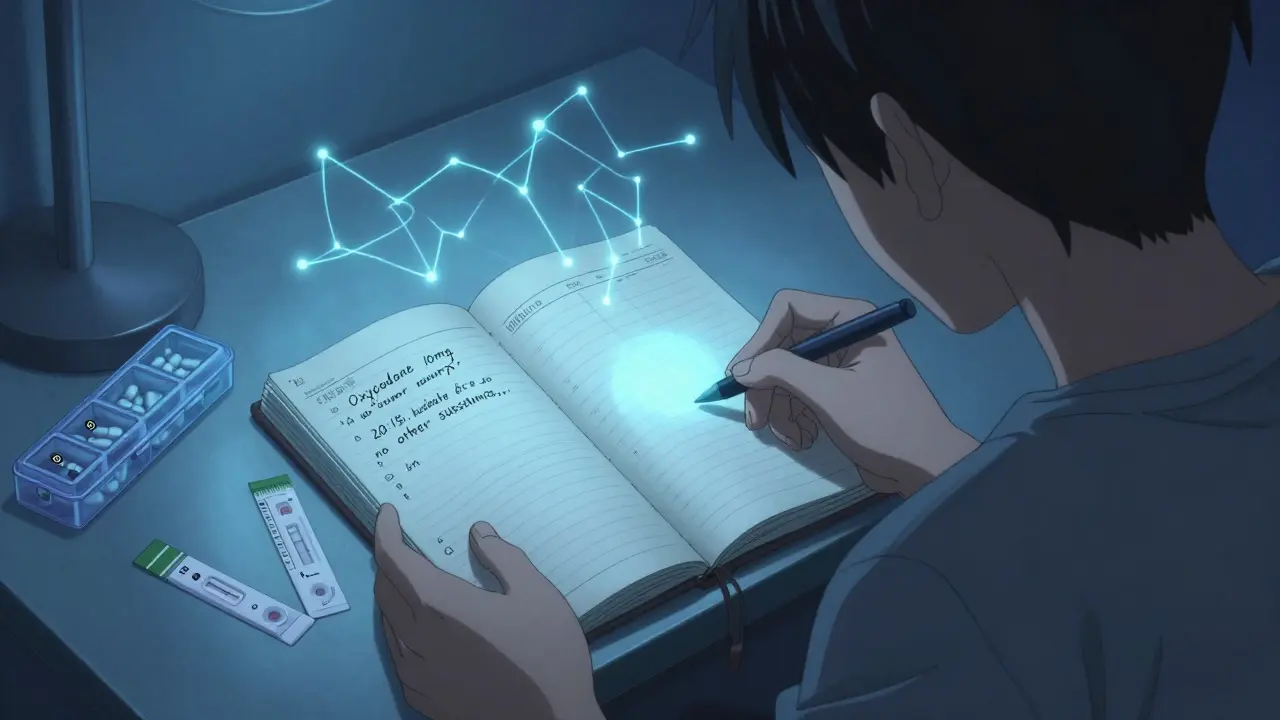
How to Use a Medication Log to Prevent Overdose Errors
- Date: 20 Dec 2025
- Categories:
- Author: David Griffiths
A simple medication log can prevent deadly overdose errors by tracking exactly what you take, when, and how much. Learn how to build one, what to include, and why it saves lives - whether you're on prescriptions or using street drugs.

How to Prevent Accidental Double-Dosing of Medications at Home
- Date: 14 Nov 2025
- Categories:
- Author: David Griffiths
Accidental double-dosing of medications at home is a leading cause of preventable overdoses. Learn practical, proven strategies-including pill organizers, digital reminders, ingredient checks, and safe storage-to protect yourself and loved ones from dangerous medication errors.