Accidental double-dosing is more common than you think
It happens quietly. Someone takes their morning pill, then gets distracted by a phone call, a visitor, or a child asking for help. Later, they look at the bottle and think, Did I take it already? So they take it again. That’s double-dosing. And it’s not just a mistake-it’s a health emergency waiting to happen.
Every day in the U.S., at least one person dies because of a medication error. Half of those happen at home. And the biggest cause? Taking the same medicine twice by accident. Older adults, kids, and households with multiple caregivers are at highest risk. The average senior takes four or five prescription drugs a day. Add in over-the-counter painkillers, vitamins, and supplements, and it’s easy to lose track.
Why double-dosing is so dangerous
Many medications have narrow safety margins. Take too much acetaminophen, and your liver can fail. Too much blood pressure medicine, and your heart rate drops dangerously low. Warfarin, a common blood thinner, can cause internal bleeding if taken twice in one day. Even something as simple as an antihistamine can lead to dizziness, confusion, or falls in older adults.
One of the scariest parts? People often don’t realize they’ve overdosed until it’s too late. A 2023 study from Children’s Healthcare of Atlanta found that 86% of emergency visits for medicine poisoning in kids involved medications taken from a family member’s cabinet-not from a child’s own prescription. That means even if you’re careful with your own pills, someone else’s medicine can still put your loved ones at risk.
Use a pill organizer-don’t just buy one, use it right
The most effective tool for preventing double-dosing is a simple pill organizer. Not the fancy ones with alarms. Just a basic weekly box with AM, noon, PM, and bedtime slots. It works because your eyes see the truth before your brain forgets it.
Here’s how to make it work:
- Fill the organizer once a week, at the same time-Sunday evening works well.
- Use a different color for each time of day (e.g., blue for morning, red for night).
- After taking a dose, leave the compartment empty. No covering, no flipping, no guessing.
WesleyLife’s 2023 survey found that 68% of seniors use weekly pill organizers. Those who used them alone cut double-dosing by 35%. But when combined with another strategy, the drop jumped to 62%.
Pro tip: Don’t refill the organizer until you’ve taken all the pills from the previous week. If you see pills left over, stop. Call your pharmacist. You may have missed a dose-or taken one twice.
Use digital reminders-but make them smart
Smartphone apps like Medisafe, MyTherapy, or even built-in calendar alerts can be game-changers. They don’t just remind you. They track what you’ve taken, sync with family members, and send alerts if you miss a dose.
But here’s the catch: 70% of people who download these apps stop using them within three weeks. Why? They’re too complicated to set up, or no one else in the house knows about them.
Fix this by:
- Setting up the app together with a family member or caregiver.
- Using the same app on two phones-one for you, one for your spouse or adult child.
- Enabling notifications for both the time of day and the actual dose taken (not just a beep, but a visual checkmark).
A 2022 study in the Journal of Medical Internet Research found that users who shared their medication tracking with someone else had 87% better adherence. That’s not just a reminder-it’s a safety net.
Never use kitchen spoons to measure liquid medicine
It sounds harmless. You don’t have the syringe. The child is crying. You just need a quick teaspoon. But a kitchen teaspoon can hold anywhere from 2.5 to 7.3 milliliters. That’s a 200% variation. For a child’s antibiotic or fever reducer, that could mean the difference between a safe dose and a toxic one.
Children’s Healthcare of Atlanta’s 2023 data shows that 41% of pediatric double-dosing cases happened because parents gave extra doses after the child spit out the first one. They didn’t know how much was actually swallowed. They didn’t have the right tool. So they gave more.
Always use:
- The syringe or cup that came with the medicine.
- A dosing cup marked in milliliters (mL), not teaspoons.
- A digital scale if you’re measuring powder or drops.
Keep these tools with your medicine. Tape the syringe to the bottle with a sticky note that says: “Only use this.”
Know what’s in your medicine-double-check ingredients
One of the most common causes of double-dosing? Taking two different pills that contain the same active ingredient.
Example: You take Tylenol for pain. Your cold medicine also has acetaminophen. You take both. You don’t realize they’re the same thing. You’ve just taken 1,000 mg extra-right at the edge of the daily limit.
EssexCare Pharmacy tracked 32% of double-dosing cases in 2023 as cases where patients didn’t know two meds had the same ingredient. That’s not their fault. Labels are confusing. Pharmacists are busy. You need to check.
Do this:
- Make a list of every medicine you take-prescription, OTC, vitamins, supplements.
- Write down the active ingredient for each (not just the brand name).
- Use a free online checker like MedlinePlus or ask your pharmacist to review it.
Keep this list on your phone and in your wallet. Update it every time you get a new prescription.
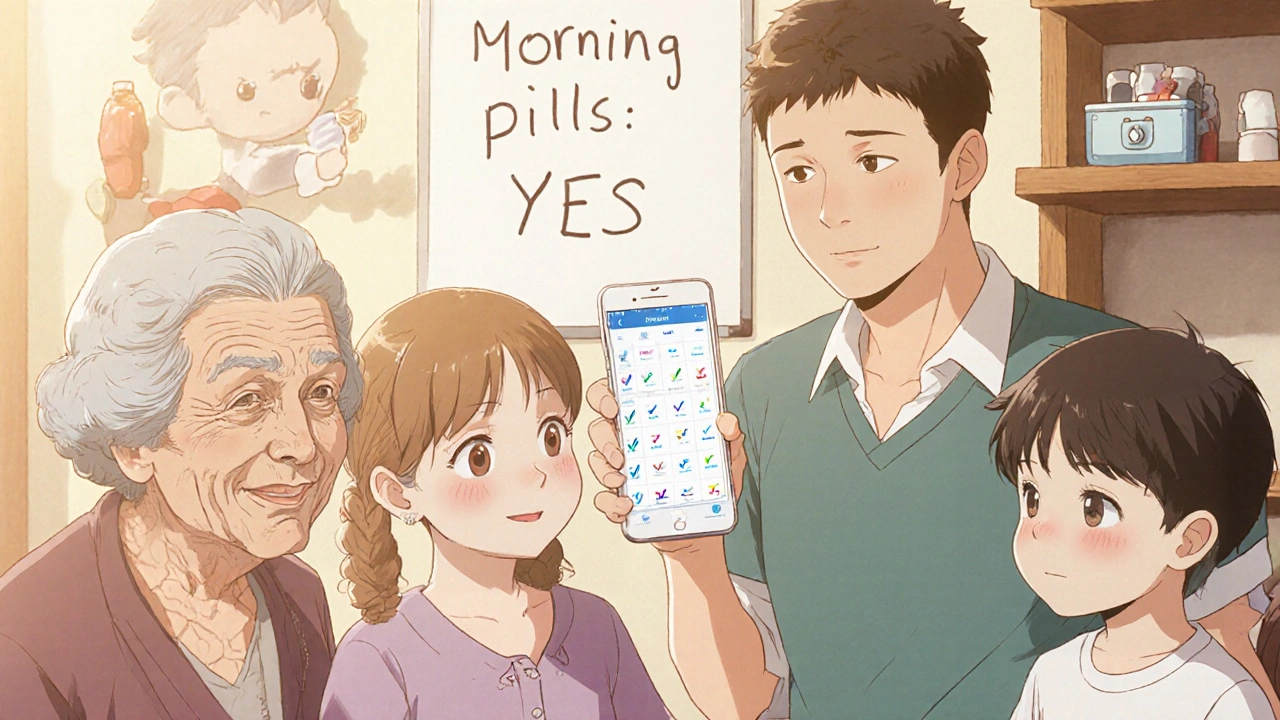
Assign one person to handle dosing
If you have kids, aging parents, or multiple caregivers in the house, the biggest risk isn’t forgetting-it’s overlap.
St. Louis Children’s Hospital found that assigning one person to give all medications cuts double-dosing by 47%. That’s not just a suggestion-it’s a rule. One person gives the medicine. One person checks the list. One person updates the app.
It doesn’t matter who. It matters that it’s consistent. In households where caregivers switched off, 62% of double-dosing incidents happened during transitions-like when Grandma came to visit or Dad got home from work.
Use a whiteboard or a shared app to write: “Morning pills given: Yes/No.” Make it visible. Make it simple.
Store medicine out of reach and out of sight
Accidental double-dosing isn’t just about forgetting. It’s about access.
Children’s Healthcare of Atlanta reports that 86% of medicine poisonings in kids involved pills taken from a family member’s cabinet. That means your medicine isn’t safe just because you take it right. It’s safe only if no one else can reach it.
Lock it up. Even if you think your kids are too young to climb, or your grandkids are too careful. A 2023 study showed that toddlers can open child-resistant caps in under 10 seconds if they’re motivated.
Use a locked medicine box. Or put it in a high cabinet with a child lock. Don’t leave pills on the bathroom counter. Don’t keep them in a purse or jacket pocket. If it’s not locked, it’s a risk.

Sync meds with daily routines
Memory fails. Habits don’t.
St. Louis Children’s Hospital found that 78% of people who successfully avoided double-dosing tied their medication to a daily habit: brushing teeth, eating breakfast, or turning off the TV at night.
Why? Routine creates automatic behavior. You don’t think about it. You just do it.
Try this:
- Take your morning pills right after you brush your teeth.
- Take your nighttime pills right before you get into bed.
- Put your pill organizer next to your coffee maker or toothbrush.
It’s not magic. It’s neuroscience. Your brain links actions together. Make the medicine part of the habit, and forgetting becomes rare.
What to do if you think you’ve double-dosed
If you realize you took two doses-don’t wait. Don’t Google it. Don’t hope it’s fine.
Call 1-800-222-1222 right away. That’s the National Poison Control Center. They’re free, confidential, and available 24/7. They’ll ask you what you took, how much, and when. Then they’ll tell you exactly what to do.
Some cases need emergency care. Others just need to wait and watch. Either way, you need expert advice-not a guess.
Keep that number saved in your phone. Write it on the fridge. Tell your family where it is.
Technology is helping-but don’t abandon the simple stuff
Smart pill dispensers that lock after a dose are now available. They cost $100-$300. In a 2023 Johns Hopkins study, they reduced double-dosing by 76%. But they’re not for everyone.
Many seniors still prefer paper lists and pill boxes. That’s okay. The goal isn’t tech-it’s safety.
The best system is the one you’ll use every day. For some, that’s a printed schedule taped to the mirror. For others, it’s an app with voice alerts. For families, it’s a shared note on their phone.
Don’t overcomplicate it. Start with one thing: a pill organizer. Then add one more: a reminder. Then one more: a list of ingredients. Build slowly. Stay consistent.
It’s not about being perfect-it’s about being protected
You don’t need to remember every pill, every time. You just need a system that catches you when you forget.
Double-dosing isn’t a sign of carelessness. It’s a sign that the system failed. And systems can be fixed.
Start today. Fill a pill box. Write down your meds. Call your pharmacist. Tell someone who helps you. You’re not just preventing a mistake. You’re preventing a crisis.




So let me get this straight-we’re trusting people to remember pills like they’re remembering to feed their goldfish? 🤦♀️ I’ve seen my grandma take her blood pressure med at 7am, then again at 11am because she ‘thought she forgot.’ She’s got a pill organizer sitting in the drawer collecting dust. And don’t even get me started on the ‘use a syringe’ thing-half the time the kid spits it out and mom just guesses. We’re not fixing systems. We’re just hoping someone remembers to breathe.