Medicare Part D: What It Covers, How It Works, and What You Need to Know
When you’re on Medicare Part D, the federal program that helps pay for prescription drugs for people enrolled in Medicare. It’s not automatic—you have to pick a plan, and the wrong choice can cost you hundreds or even thousands extra every year. This isn’t just about getting your pills covered. It’s about understanding how your plan’s drug formulary, the list of medications your plan covers works, what tier your meds are on, and whether your pharmacy is in-network. Many people assume all Part D plans are the same, but they’re not. One plan might cover your insulin at $10 a month, while another charges $80—even if they’re both called "Medicare Part D."
There’s also the donut hole, the coverage gap where you pay more out of pocket after spending a certain amount on drugs. It used to be a big financial trap, but now discounts and protections make it less dangerous than before. Still, if you take multiple prescriptions, you need to track your spending carefully. Some plans offer extra help if your income is low, but you have to apply for it—you won’t get it automatically. And don’t forget about out-of-pocket costs, what you pay before insurance kicks in, including deductibles, copays, and coinsurance. These can add up fast, especially if you’re on expensive meds like those for autoimmune diseases or cancer.
You’ll also find that some drugs require prior authorization or step therapy. That means your doctor has to prove you tried cheaper options first, or your plan won’t pay. This affects medications like GLP-1 agonists for weight loss, certain biologics for uveitis, or even common painkillers like celecoxib if they’re used long-term. It’s not just about getting the right drug—it’s about navigating the system that decides if you can get it at all.
Medicare Part D connects to everything else in your health journey. If you’re managing diabetes and methotrexate, or taking donepezil for memory, or using antifungals for skin issues, your Part D plan determines whether you can afford them. It’s tied to how you refill prescriptions, whether your pharmacy uses EHR systems to avoid double-dosing, and even whether you can stick to your medication action plan. This collection of articles covers the real-world side of taking meds under Medicare—how to avoid errors, how to talk to your pharmacist about generics, how patent laws affect drug prices, and how to spot when your plan’s rules are working against you. You don’t need to be an expert to get the most out of your coverage. You just need to know what questions to ask.
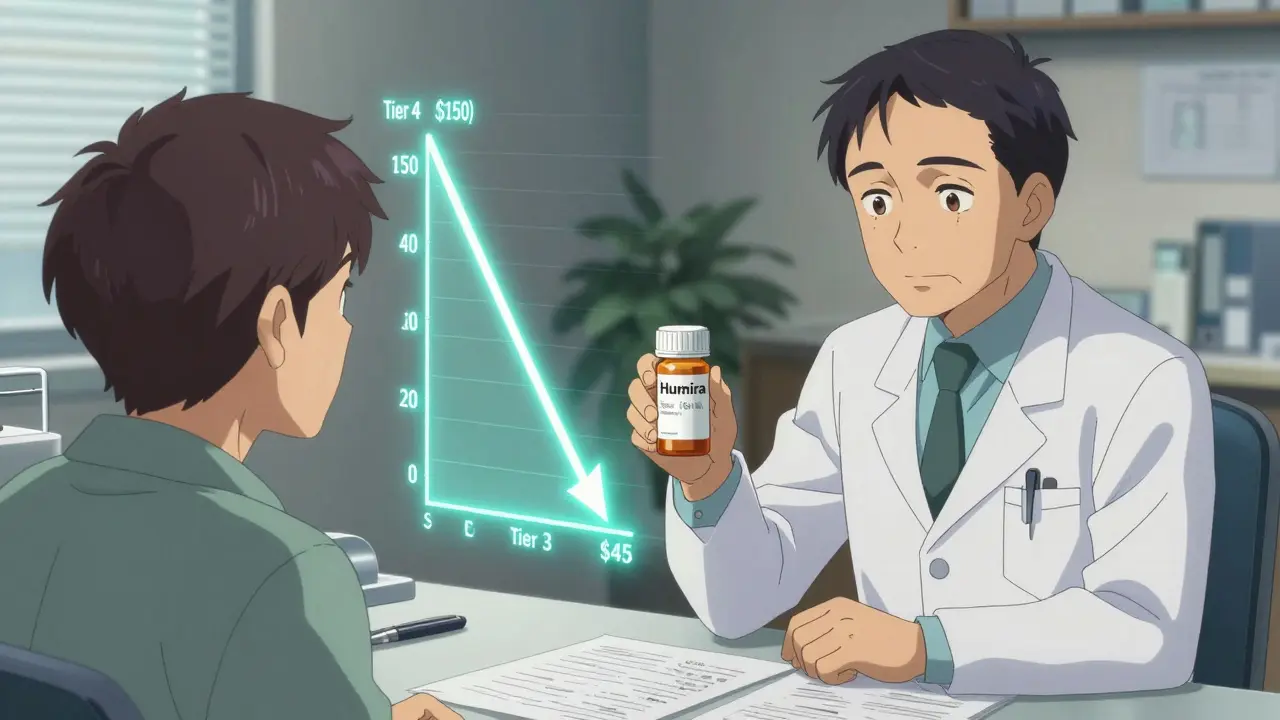
How to Use Tier Exceptions to Lower Your Medication Copays
- Date: 5 Jan 2026
- Categories:
- Author: David Griffiths
Learn how to request a tier exception to lower your medication copays. Move high-cost drugs to lower tiers and save hundreds per year with simple steps and doctor-supported documentation.

Extra Help Program for Low-Income Seniors: How to Qualify for Prescription Drug Savings
- Date: 27 Nov 2025
- Categories:
- Author: David Griffiths
Learn how low-income seniors can qualify for the Medicare Extra Help Program to cut prescription drug costs to just a few dollars per pill. Get the 2025 income limits, application steps, and hidden benefits you might not know about.