Uveitis Treatment: What Works, What to Avoid, and How to Manage It
When the middle layer of your eye—the uvea, the pigmented layer between the sclera and retina that includes the iris, ciliary body, and choroid. Also known as intermediate uvea, it plays a key role in eye health and blood flow.—becomes inflamed, you’re dealing with uveitis. It’s not just redness or discomfort; untreated uveitis can lead to glaucoma, cataracts, or even vision loss. The good news? Most cases respond well to treatment if caught early. This isn’t something you should ignore or try to outwait. Uveitis can be caused by infections, autoimmune diseases like rheumatoid arthritis or sarcoidosis, trauma, or sometimes, no clear reason at all. But no matter the trigger, the goal is the same: reduce inflammation fast and protect your sight.
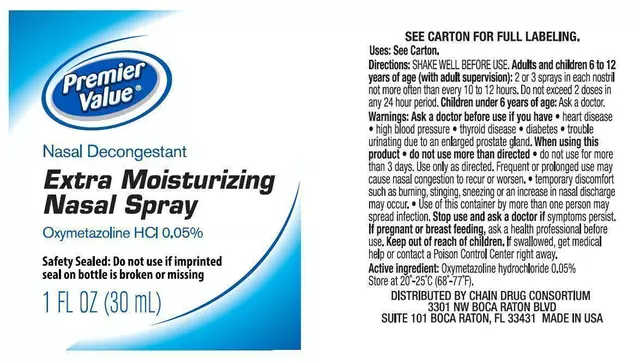
Standard corticosteroids, powerful anti-inflammatory drugs used to calm immune responses in the eye. Also known as steroids, they are the first-line defense in most uveitis cases. come in the form of eye drops, pills, or injections—depending on how deep the inflammation goes. For front-of-eye uveitis, drops like prednisolone are often enough. But if it’s in the back of the eye or spreading, you might need oral steroids or even a shot near the eye. The catch? Long-term steroid use brings risks: higher eye pressure, cataracts, and bone thinning. That’s why doctors often turn to immunosuppressants, medications that lower immune system activity to prevent recurring inflammation. Also known as disease-modifying drugs, they help reduce steroid dependence over time. like methotrexate or mycophenolate. These aren’t quick fixes—they take weeks to kick in—but they’re essential for chronic or recurrent cases. You’ll need regular blood tests to monitor liver and kidney function. And if an infection like herpes or tuberculosis is behind the uveitis, antibiotics or antivirals become part of the plan. No one-size-fits-all here. Your treatment is shaped by your age, medical history, and how the inflammation behaves.
What you don’t do matters just as much as what you do. Avoid rubbing your eyes. Skip over-the-counter redness-relief drops—they mask symptoms but don’t treat the root problem. And never delay seeing an eye specialist if your vision blurs, light becomes painful, or redness worsens. Uveitis can sneak up quietly, especially in younger people with autoimmune conditions. The posts below give you real-world insight: how people manage flare-ups, what side effects to expect from meds, when to push for a second opinion, and how lifestyle choices like quitting smoking or managing stress can influence recovery. You’ll find practical advice on monitoring symptoms at home, understanding lab results, and working with your care team to balance effectiveness with safety. This isn’t about guesswork. It’s about knowing what works, why it works, and how to stay in control.

Autoimmune Uveitis: Understanding Eye Inflammation and Steroid-Sparing Treatments
- Date: 24 Nov 2025
- Categories:
- Author: David Griffiths
Autoimmune uveitis is a serious eye condition caused by the immune system attacking the eye. Steroid-sparing therapies like Humira, methotrexate, and cyclosporine help control inflammation without the long-term risks of steroids.