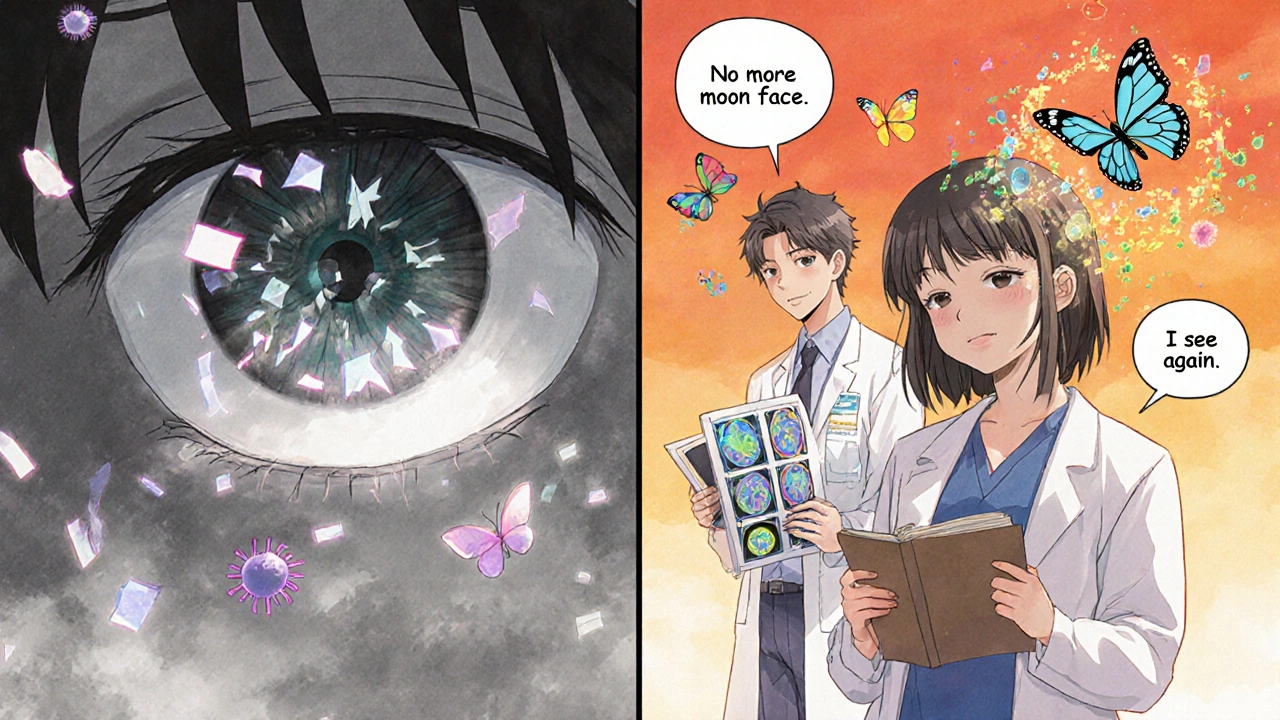
When your eyes feel red, sore, and blurry-like you’ve been staring at a bright light too long-it’s easy to brush it off as fatigue or allergies. But if those symptoms stick around, or come back again and again, it could be something more serious: autoimmune uveitis. This isn’t just a simple eye infection. It’s your own immune system attacking the middle layer of your eye, causing inflammation that can quietly steal your vision if left unchecked.
What Exactly Is Autoimmune Uveitis?
Uveitis means inflammation of the uvea-the middle layer of your eye that includes the iris, ciliary body, and choroid. In autoimmune uveitis, your immune system mistakes parts of your eye for foreign invaders and starts attacking them. It’s not caused by an injury or bacteria. It’s an internal mistake, one that often links to other autoimmune diseases like rheumatoid arthritis, lupus, Crohn’s disease, or ankylosing spondylitis.People with this condition might notice:
- Redness in one or both eyes
- Pain or aching behind the eye
- Blurred or cloudy vision
- Sensitivity to light (photophobia)
- Floaters-spots or strings drifting across your vision
- Headaches that seem tied to eye pressure
Symptoms can hit fast or creep in slowly. Sometimes, only one eye is affected at first. But without treatment, the inflammation doesn’t just go away. It can lead to cataracts, glaucoma, retinal detachment, or permanent vision loss. That’s why getting checked by an ophthalmologist within 24 hours of symptoms is critical.
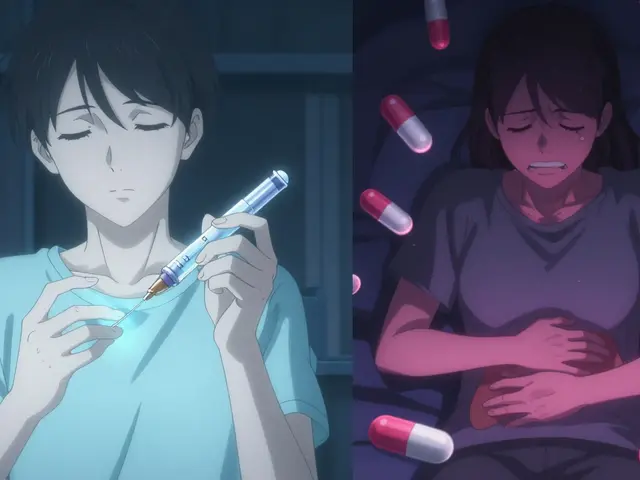
Why Steroids Are the First Line-But Not the Long-Term Solution
When uveitis flares up, doctors reach for corticosteroids fast. These powerful anti-inflammatory drugs-given as eye drops, injections around the eye, or pills-can calm the inflammation quickly. For many people, this is life-changing. Vision clears up. Pain fades. It feels like a miracle.But here’s the catch: steroids aren’t meant to be taken for months or years. Long-term use brings its own set of dangers:
- Cataracts-clouding of the lens, requiring surgery
- Glaucoma-increased eye pressure that damages the optic nerve
- Bone thinning, weight gain, high blood sugar, mood swings, and weakened immunity
For someone with recurring uveitis, staying on steroids is like trading one problem for another. That’s where steroid-sparing therapy comes in.
Steroid-Sparing Therapy: What It Is and How It Works
Steroid-sparing therapy means using other drugs to control inflammation so you can reduce or stop steroids altogether. These aren’t quick fixes. They work over weeks and months to retrain your immune system so it stops attacking your eye.The most common options include:
- Methotrexate: An older immunosuppressant, often used for rheumatoid arthritis. It’s taken weekly as a pill or injection and has decades of use in uveitis.
- Cyclosporine: Another immunosuppressant that targets specific immune cells. It requires regular blood tests to monitor kidney function.
- Adalimumab (Humira): The first FDA-approved biologic specifically for non-infectious uveitis. It blocks TNF-alpha, a protein that drives inflammation. Many patients see fewer flares and less steroid dependence.
- Infliximab: Used successfully in children with uveitis, with studies showing high response rates and reduced steroid needs.
These drugs don’t work the same for everyone. Some people respond quickly. Others need to try two or three before finding one that helps. That’s why treatment has to be personalized-based on the type of uveitis (anterior, intermediate, posterior), whether it’s linked to another autoimmune disease, and how severe it is.

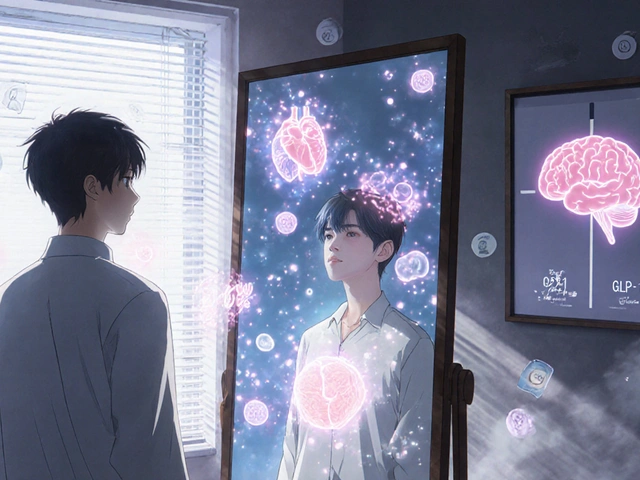
Why Collaboration Between Doctors Matters
Autoimmune uveitis doesn’t live in the eye alone. It’s often a sign of a larger immune system problem. That’s why seeing both an ophthalmologist and a rheumatologist isn’t optional-it’s essential.An ophthalmologist can track eye damage with tools like optical coherence tomography (OCT), fluorescein angiography, and tonometry. But only a rheumatologist can run the right blood tests to check for lupus, sarcoidosis, or ankylosing spondylitis. Together, they can tell if this is truly autoimmune-or if it’s caused by an infection like tuberculosis or Lyme disease. Mistake that, and you could give someone immunosuppressants when they need antibiotics. That’s dangerous.
Specialized uveitis clinics have grown from just 15 in 2010 to over 50 across the U.S. by 2023. These centers bring both specialists under one roof, making coordination easier and treatment faster.
What Patients Experience When Switching to Steroid-Sparing Therapy
Many patients describe the transition as a relief-but not without challenges. Once they start methotrexate or Humira, their eye symptoms often stabilize. They can cut their steroid dose in half, then drop it entirely. No more moon face. No more sleepless nights from high blood sugar. Their energy returns. They can go back to work, play with their kids, drive without fear.But there’s a trade-off. These drugs suppress the immune system. That means a simple cold can turn into something worse. You need to avoid crowds during flu season. You may need vaccines before starting treatment. Blood tests every few weeks become routine. Some people feel anxious about being “immunocompromised.”
Still, most say the trade-off is worth it. One patient in a 2023 study said, “I’d rather take a pill every week than live with blurry vision and the fear of going blind.”
What’s Next? The Future of Uveitis Treatment
The FDA’s approval of Humira in 2016 was a turning point. But it’s just the beginning. Researchers are now testing drugs that target other parts of the immune system-like interleukin inhibitors (IL-6, IL-17) and JAK inhibitors. Early results show promise for patients who don’t respond to TNF blockers.There’s also growing interest in personalized medicine. Scientists are looking at genetic markers and blood proteins that might predict who will respond to which drug. In the next five years, we may see blood tests that tell your doctor, “You’re more likely to respond to adalimumab than methotrexate.”
Laser treatments, cryotherapy, and surgery still have a role-but only for complications. The real shift is toward smarter, safer drugs that stop inflammation before it starts.
What You Should Do If You Suspect Uveitis
If you’ve had eye redness, pain, or vision changes for more than a few days:- See an ophthalmologist immediately. Don’t wait. Delayed treatment increases the risk of permanent damage.
- Ask if your uveitis might be autoimmune. Mention any history of arthritis, skin rashes, bowel issues, or other autoimmune conditions.
- Request a referral to a rheumatologist if you haven’t had one already.
- Ask about steroid-sparing options-even if you’re just starting steroids. Planning ahead saves you from long-term side effects.
- Keep a symptom journal. Note when flares happen, what triggers them, and how your vision changes.
Autoimmune uveitis isn’t common-it affects fewer than 200,000 people in the U.S. But for those who have it, the impact is huge. The good news? We have better tools now than ever before. With the right team, the right drugs, and the right timing, most people can protect their vision and live full lives-without relying on steroids forever.
Can autoimmune uveitis be cured?
There’s no cure for autoimmune uveitis, but it can be managed effectively. With the right treatment plan-especially steroid-sparing therapy-many people achieve long-term remission and avoid vision loss. The goal isn’t to eliminate the disease completely, but to control it so it doesn’t damage your eyes.
How long does steroid-sparing therapy take to work?
It usually takes 6 to 12 weeks for drugs like methotrexate or Humira to show full effect. That’s why doctors don’t stop steroids right away. They gradually reduce the steroid dose as the new drug kicks in. Patience is key-rushing the process can lead to a flare-up.
Are biologics like Humira safe for long-term use?
Biologics carry risks, including increased chance of infections and rare cases of neurological or liver issues. But for people with severe, recurrent uveitis, the benefits usually outweigh the risks. Regular blood tests and monitoring by your doctor help catch problems early. Many patients use these drugs safely for years.
Can I still wear contact lenses if I have uveitis?
During active inflammation, you should avoid contact lenses. They can trap irritants, increase infection risk, and make symptoms worse. Once inflammation is fully controlled and your doctor gives the green light, you may be able to wear them again-but always follow strict hygiene rules.
Does diet or lifestyle affect autoimmune uveitis?
No specific diet has been proven to cure or prevent uveitis flares. But maintaining a healthy weight, not smoking, and managing stress can support overall immune health. Some patients with linked conditions like Crohn’s or psoriasis benefit from anti-inflammatory diets-but always talk to your doctor before making big changes.
What if I can’t afford steroid-sparing drugs?
Biologics like Humira are expensive, but many pharmaceutical companies offer patient assistance programs. Your doctor’s office can help you apply. Generic versions of older drugs like methotrexate are affordable and still effective. Don’t skip treatment because of cost-there are options.
Can uveitis come back after stopping treatment?
Yes, flares can happen even after years of remission. That’s why regular eye checkups-even if you feel fine-are crucial. Your doctor may recommend follow-ups every 3 to 6 months. Early detection of a flare means quicker treatment and less damage.
Autoimmune uveitis doesn’t define you. But how you respond to it can change everything. With the right care, you don’t have to choose between vision and side effects. You can have both-clear sight and a full life.

Okay but have yall seen the price of Humira lately? I had to sell a kidney just to get my monthly dose and now my vision is clear but my bank account is crying