tTG Antibodies: What They Mean for Celiac Disease and Autoimmune Health
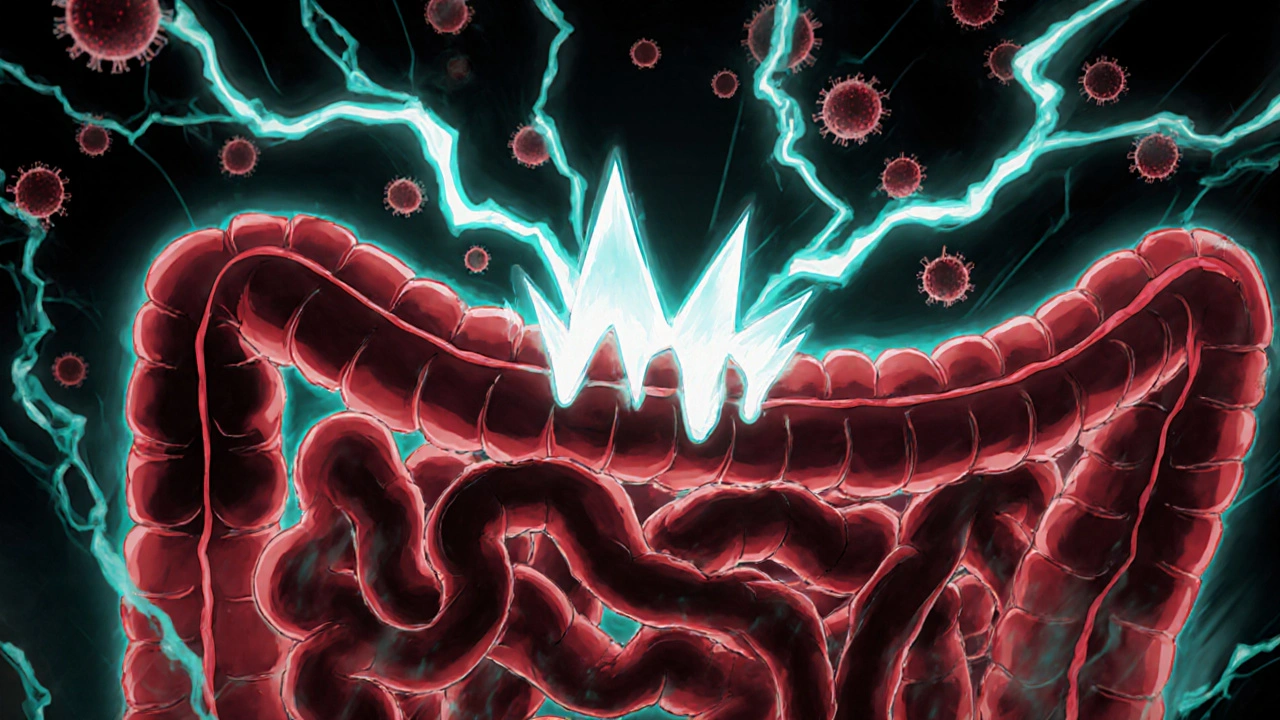
When your body mistakes gluten for a threat, it may start producing tTG antibodies, antibodies that target tissue transglutaminase, an enzyme in the small intestine. Also known as anti-tTG, these immune proteins are one of the most reliable signs of celiac disease—a condition where eating gluten damages the gut lining. Unlike temporary food sensitivities, tTG antibodies don’t go away just because you feel better. They stick around as long as gluten is in your system, making them a critical tool for diagnosis and monitoring.
These antibodies don’t appear out of nowhere. They’re tied to a specific autoimmune reaction triggered by gluten in people with certain genes. That’s why tTG antibodies are rarely found in people without celiac disease—or those who’ve already gone gluten-free. When levels are high, it’s not just a lab result. It’s your immune system actively attacking your own intestine. That’s why doctors pair tTG antibody tests with other checks, like biopsy, a tissue sample from the small intestine used to confirm intestinal damage, or genetic testing, checking for HLA-DQ2 and HLA-DQ8 genes that make celiac disease possible. You can have high tTG antibodies without a biopsy, but the combo gives you the full picture.
People often confuse tTG antibodies with general gluten sensitivity. But here’s the difference: gluten sensitivity doesn’t usually raise these antibodies. If your tTG levels are normal, celiac disease is unlikely—even if you feel better off gluten. But if they’re high, skipping gluten isn’t just a diet choice—it’s a medical necessity. Left unchecked, ongoing antibody activity can lead to nutrient deficiencies, osteoporosis, or even rare intestinal cancers. That’s why catching it early matters.
What you’ll find in the posts below isn’t just theory. It’s real-world guidance from people who’ve been there. You’ll see how tTG antibodies connect to other autoimmune conditions like uveitis and rheumatoid arthritis, how medications like methotrexate can affect them, and why some people still have elevated levels even after going gluten-free. This isn’t about guessing. It’s about understanding what your body is telling you—and what to do next.
Celiac Disease: How Gluten Triggers Autoimmune Damage and What Diet Really Requires
- Date: 28 Nov 2025
- Categories:
- Author: David Griffiths
Celiac disease is an autoimmune disorder triggered by gluten, causing intestinal damage. Learn how it works, why a strict gluten-free diet is essential, and what new treatments are emerging.