When someone with celiac disease eats bread, pasta, or even a spoonful of soy sauce, their immune system doesn’t just react-it attacks. Not the food. Not the bacteria. But their own small intestine. This isn’t a food allergy. It’s an autoimmune war, triggered by a protein called gluten, and it’s happening in about 1 in 100 people worldwide. For decades, the only solution was simple: avoid gluten completely. But understanding celiac disease goes far beyond just reading labels. It’s about how your genes, your gut lining, and your immune system team up to turn a common food into a silent destroyer.
How Gluten Turns Into an Enemy Inside Your Body
Gluten isn’t just any protein. It’s the sticky stuff in wheat, barley, and rye that gives bread its chew. But for people with celiac disease, it’s a trigger for chaos. The problem starts when gluten survives digestion. Most proteins break down easily. Gluten doesn’t. A stubborn fragment called the 33-mer gliadin slips through the gut lining, thanks to a protein called zonulin that loosens the tight junctions between cells. Once it’s past the barrier, tissue transglutaminase 2 (TG2)-an enzyme normally involved in wound healing-starts modifying it. It snips off certain parts and adds negative charges, making the gluten fragment look like a threat to the immune system. This is where genetics come in. If you carry HLA-DQ2 or HLA-DQ8 genes (about 30% of people do), your immune cells are wired to recognize these altered gluten pieces. Antigen-presenting cells grab them and show them to CD4+ T cells. These T cells then scream for help, releasing massive amounts of interferon-gamma and interleukin-21. That’s not a normal response. That’s a full-blown autoimmune attack. The result? The finger-like projections in your small intestine-called villi-start to flatten. Nutrients can’t be absorbed. Diarrhea, fatigue, weight loss, and even anemia follow. A 2024 study from McMaster University changed everything. Scientists found that the gut lining itself isn’t just a passive victim-it can actively start the immune response. Cells in the epithelium, when expressing the same HLA-DQ2 molecules found in immune cells, can present gluten to T cells. That means your gut isn’t just getting damaged-it’s helping cause the damage. This discovery is rewriting textbooks and opening doors to new treatments.It’s Not Just Gluten Sensitivity
Many people think if they feel better off gluten, they have celiac disease. They don’t. Non-celiac gluten sensitivity (NCGS) is real, but it’s not the same. While celiac affects 1-4% of people globally, NCGS is estimated between 0.5% and 13%. The big difference? No autoimmune damage. No villous atrophy. No specific antibodies. In celiac disease, your blood will show high levels of anti-tissue transglutaminase (tTG) antibodies-98% sensitive and 95% specific. That’s a gold-standard test. In NCGS, blood tests come back normal. You might feel bloated, tired, or foggy after eating gluten, but your intestine looks fine under the microscope. And here’s the kicker: people with NCGS often tolerate small amounts of gluten without long-term harm. For someone with celiac, even a crumb can keep the immune system firing for weeks. The immune signatures are different too. Celiac patients show strong IgG3 responses, suggesting repeated, unrelenting activation. NCGS patients have more varied IgG patterns, possibly indicating their bodies are trying to calm inflammation, not destroy tissue. That’s why misdiagnosis is common-and dangerous.The Gluten-Free Diet: What It Really Means
The only proven treatment for celiac disease is a lifelong, strict gluten-free diet. Not “mostly.” Not “most of the time.” Total. Absolute. No exceptions. The legal limit for “gluten-free” labeling? 20 parts per million (ppm). That’s one drop of soy sauce in a full bathtub of water. But even that tiny amount can trigger damage in sensitive individuals. A 2023 study found that 30% of people with celiac still have intestinal damage after years on a gluten-free diet-not because they’re cheating, but because of hidden exposure. Cross-contamination is the silent killer. A toaster used for regular bread? A knife that cut a bagel? A shared fryer? These aren’t myths. A 2022 survey showed 67% of celiac patients had experienced cross-contamination in restaurants. Even gluten-free oats can be contaminated if processed in the same facility as wheat. Getting started means a full pantry reset. Replace flour, breadcrumbs, sauces, and seasonings. Look for certified gluten-free labels. Learn to spot hidden gluten: malt flavoring, hydrolyzed vegetable protein, modified food starch (unless labeled gluten-free), and even some medications. One patient in Melbourne told me she didn’t realize her daily multivitamin contained wheat starch until her follow-up biopsy showed no healing. Cost is a real barrier. Gluten-free products cost, on average, 242% more than regular versions. A box of gluten-free pasta might be $8 instead of $2.50. That’s not just inconvenient-it’s unfair.
What Happens After You Go Gluten-Free?
The good news? Most people feel better fast. A 2023 survey of over 15,000 celiac patients found 89% saw major improvement within six months. Fatigue lifts. Bloating disappears. Brain fog clears. The body is designed to heal-if you stop the attack. But healing takes time. In children, villi can recover in 3-6 months. In adults, it often takes 1-2 years. A follow-up endoscopy is the only way to confirm healing. One patient, after five years of strict dieting, finally had a biopsy in January 2024 that showed complete mucosal recovery. That’s the goal. Still, 42% of patients report ongoing symptoms. Why? Cross-contamination is the top reason. But there’s also the possibility of other triggers-like infections, stress, or an imbalanced gut microbiome. Research now shows that 78% of celiac patients have a unique gut bacteria profile compared to healthy people. Are these microbes causing harm, or are they a result of the damaged gut? Scientists are still figuring it out. Nutrient deficiencies are common at diagnosis. Iron deficiency? Affects 33%. Vitamin D? 47%. Calcium? 39%. That’s why blood tests after diagnosis aren’t optional-they’re essential. Supplements may be needed for months or even years until the gut fully heals.What’s on the Horizon?
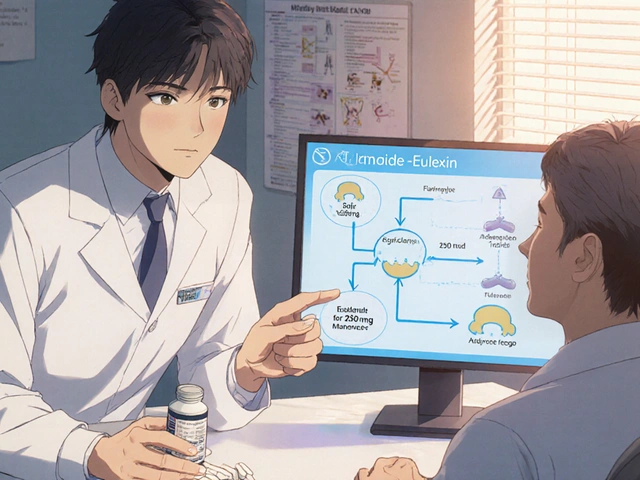
The gluten-free diet works-but it’s a burden. No one should have to live like that forever. That’s why new treatments are in the pipeline. Nexvax2, a vaccine-like therapy, is designed to retrain the immune system to ignore gluten. It completed Phase 2 trials in late 2023 with a 42% drop in symptoms. Latiglutenase is an enzyme pill that breaks down gluten in the stomach before it reaches the intestine. In trials, it cut symptoms by 37%. And TAK-101, a nanoparticle treatment, showed a 63% reduction in intestinal damage by teaching the immune system to tolerate gluten. These aren’t cures yet. But they’re proof that science is catching up. By 2027-2030, combination therapies may allow people to eat gluten occasionally without damage. For now, though, the diet remains the only shield.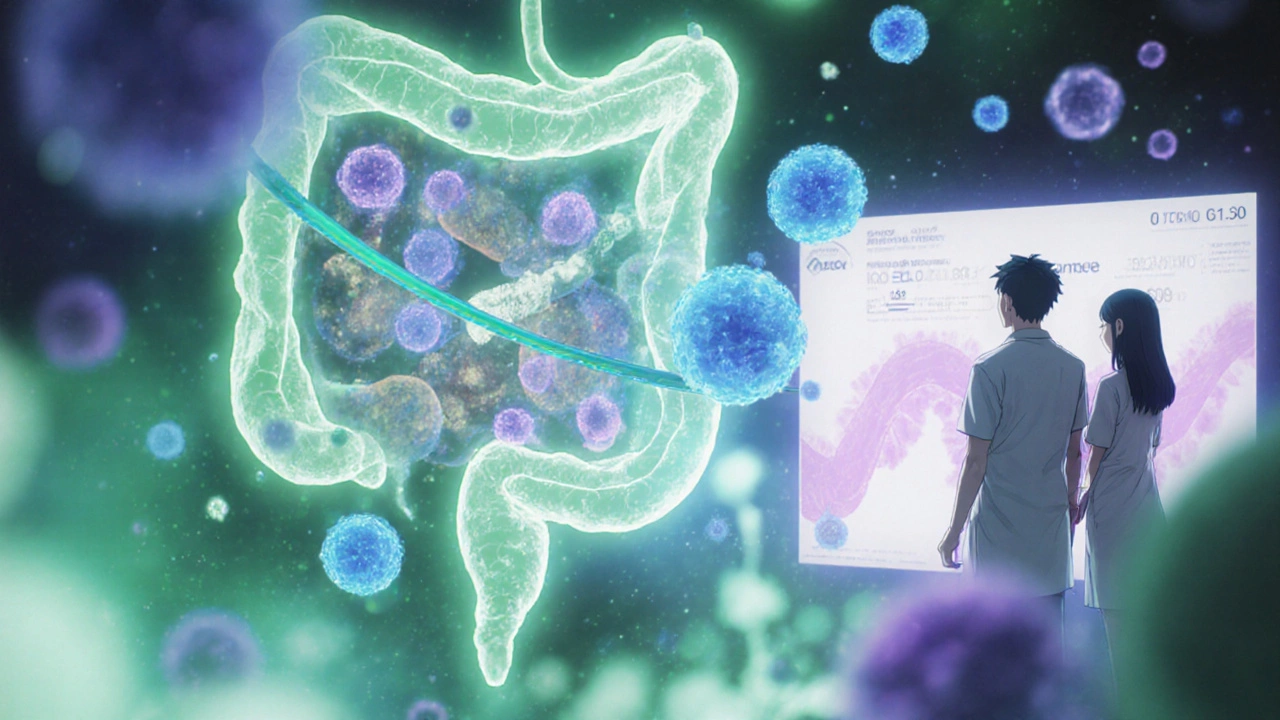
Living With It: Real Tips From Real People
The emotional toll is heavy. 58% of patients say dietary restrictions hurt their quality of life. Social events, family dinners, travel-it all becomes stressful. One Reddit user wrote: “It took me seven years to get diagnosed. By then, I’d lost friends who didn’t understand why I couldn’t just have a bite of pizza.” Here’s what works:- Keep a gluten-free emergency snack in your bag-nuts, fruit, rice cakes.
- Use a separate toaster, cutting board, and colander at home. Studies show this cuts cross-contamination by 85%.
- Use apps like Find Me Gluten Free. It’s rated 4.7 stars by 185,000 users.
- Call restaurants ahead. Ask if they have a gluten-free protocol, not just “we have GF options.”
- Check medications with your pharmacist. Only 37% of prescription drugs list gluten content.
Testing and Diagnosis: Don’t Skip This Step
Never start a gluten-free diet before testing. If you cut gluten, your blood tests and biopsy will look normal-even if you have celiac. That’s how you get misdiagnosed. The standard path: First, a blood test for tTG-IgA antibodies. If positive, a biopsy of the small intestine confirms it. Genetic testing for HLA-DQ2/DQ8 can rule celiac out with 99% accuracy-if you don’t have the genes, you won’t get the disease. And yes, it’s worth it. Delayed diagnosis averages 6.7 years. That’s over half a decade of unnecessary damage to your body.Can celiac disease develop later in life?
Yes. Celiac disease can appear at any age, even in your 60s. It’s not just a childhood condition. Many people are diagnosed after decades of unexplained symptoms like fatigue, joint pain, or osteoporosis. The trigger could be stress, surgery, pregnancy, or an infection. Once the immune system starts reacting to gluten, the damage begins-even if you’ve eaten wheat your whole life.
Is a gluten-free diet healthy if you don’t have celiac disease?
Not necessarily. Gluten-free processed foods are often higher in sugar, fat, and calories, and lower in fiber, iron, and B vitamins. Unless you have celiac disease, non-celiac gluten sensitivity, or a wheat allergy, there’s no proven health benefit to avoiding gluten. Cutting it out without medical reason can lead to nutrient gaps and unnecessary expense.
Can you outgrow celiac disease?
No. Celiac disease is a lifelong autoimmune condition. Once diagnosed, you must avoid gluten permanently. Even if you feel fine, eating gluten will continue to damage your intestines and increase your risk for other autoimmune disorders, osteoporosis, and certain cancers. There’s no cure yet, and no evidence that the immune system ever forgets how to attack gluten.
Do oats cause problems for people with celiac disease?
Pure, uncontaminated oats are safe for most people with celiac disease. But most commercial oats are processed in facilities that handle wheat, barley, or rye. That’s why you must only eat oats labeled “gluten-free.” Even then, a small percentage of people react to avenin, a protein in oats that’s similar to gluten. If you’re unsure, talk to your doctor before adding oats to your diet.
Why do some people still have symptoms after going gluten-free?
The most common reason is accidental gluten exposure-cross-contamination in kitchens, restaurants, or medications. Other causes include lactose intolerance (common after intestinal damage), SIBO (small intestinal bacterial overgrowth), or another autoimmune condition like thyroid disease. If symptoms persist, see a specialist. A repeat biopsy or blood test can tell you if your gut is healing.
For now, the gluten-free diet remains the only tool we have to stop the autoimmune fire. But with new therapies on the horizon, the future looks less like a lifetime of fear-and more like a return to normalcy.



gluten is just a scam lol 🤡 big agri made this up to sell you $10 bread