Tacrolimus vs Cyclosporine: How They Stack Up
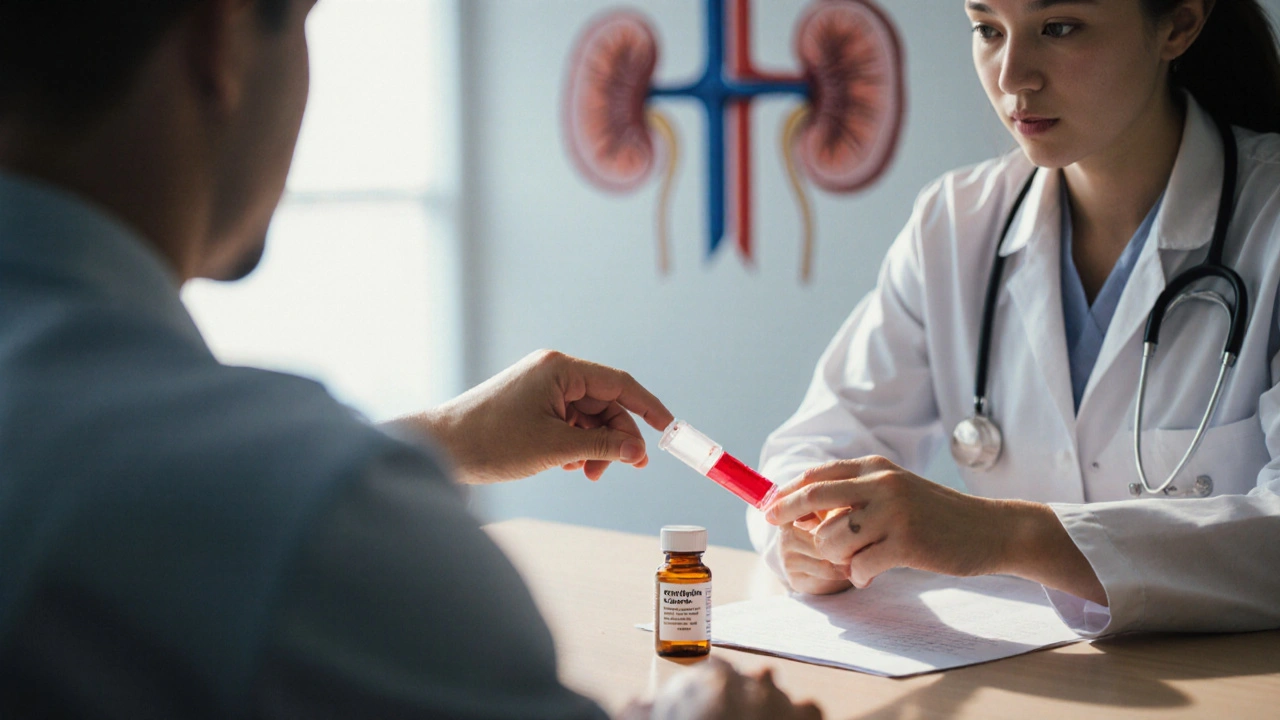
When talking about Tacrolimus vs Cyclosporine, the side‑by‑side look at two calcineurin‑inhibiting immunosuppressants. Also known as tacrolimus and cyclosporine comparison, this topic matters to anyone facing organ‑transplant decisions or chronic skin‑condition treatment. The first drug, Tacrolimus, a macrolide that blocks T‑cell activation and is used for kidney, liver, and heart transplants as well as eczema, arrived on the market in the late 1990s and quickly became a go‑to for patients needing tight immune control. Its counterpart, Cyclosporine, a cyclic peptide discovered in the 1970s, famous for preventing organ rejection and for treating psoriasis, set the stage for modern immunosuppression. Both belong to the broader class of Calcineurin inhibitors, agents that stop the enzyme calcineurin from activating immune cells, thus reducing the chance of graft loss. Because they share a mechanism, they also share many monitoring needs, but the nuances in potency, side‑effect profile, and dosing make the comparison worth a deep dive.
Key Differences at a Glance
The first semantic triple is clear: Tacrolimus vs Cyclosporine compares two drugs that suppress the immune system to prevent organ rejection. The second triple adds context: Organ transplant, a medical procedure where a failing organ is replaced by a donor organ, relies heavily on immunosuppression for success requires careful drug selection. The third triple links to disease management: Atopic dermatitis, a chronic inflammatory skin condition often treated with topical tacrolimus when steroids aren’t suitable benefits from the same drug class. When you compare potency, tacrolimus is roughly three to five times more potent than cyclosporine on a weight basis, meaning lower doses achieve the same immunosuppressive effect. This higher potency translates into tighter blood‑level control: tacrolimus levels are usually kept between 5‑15 ng/mL, while cyclosporine targets 100‑300 ng/mL. Monitoring frequency differs too—tacrolimus often needs weekly checks early on, whereas cyclosporine can be spaced out a bit longer after stabilization. Side‑effects create another semantic link. Both drugs can cause nephrotoxicity, but tacrolimus more commonly triggers neuro‑toxic symptoms like tremors or headaches, whereas cyclosporine is notorious for gum hyperplasia and hirsutism. Metabolic impacts also diverge: cyclosporine tends to raise cholesterol and triglycerides, while tacrolimus has a milder lipid effect but can increase blood sugar in susceptible patients. These distinctions matter for clinicians tailoring therapy to a patient’s existing health profile. Cost is a practical factor. In many markets, tacrolimus is priced higher due to newer patents, yet insurance formularies often favor cyclosporine for first‑line transplant protocols because of its longer track record. The decision matrix—efficacy, side‑effect tolerance, monitoring burden, and cost—forms a fourth semantic triple: Therapeutic decision‑making, the process of weighing drug attributes to choose the best immunosuppressant for a patient sits at the heart of the comparison. Overall, tacrolimus shines when a clinician needs high potency with fewer steroid‑related skin side‑effects, especially in dermatology. Cyclosporine remains a solid choice for patients who can tolerate its cosmetic side‑effects and when cost constraints dominate.
Below you’ll find a curated list of articles that dig into each of these angles—mechanism, dosing strategies, side‑effect management, and real‑world case studies. Whether you’re a transplant coordinator, a dermatologist, or a patient looking to understand why your doctor chose one over the other, the posts ahead break down the science into clear, actionable advice. Dive in to see how the nuances we’ve highlighted play out in practice, and pick the insights that match your situation.
Cyclosporine (Imusporin) vs Alternatives: Detailed Comparison
- Date: 10 Oct 2025
- Categories:
- Author: David Griffiths
A comprehensive comparison of Imusporin (cyclosporine) with its main alternatives, covering efficacy, side effects, monitoring and how to choose the right drug.