Immunosuppressant Drug Selector
Recommended Immunossuppressant:
| Drug | Drug Class | Typical Indication | Primary Advantage | Major Drawback |
|---|---|---|---|---|
| Cyclosporine | Calcineurin inhibitor | Kidney, liver, heart transplant | Proven long-term efficacy | Nephrotoxicity, cosmetic side effects |
| Tacrolimus | Calcineurin inhibitor | Kidney transplant (preferred) | Lower chronic kidney damage | Diabetes, neurotoxicity |
| Sirolimus | mTOR inhibitor | Adjunct to CNI, coronary-artery stent patients | No nephrotoxicity | Delayed wound healing, hyperlipidemia |
| Mycophenolate mofetil | Antimetabolite | Maintenance therapy with CNI | Low blood-pressure impact | GI upset, infection risk |
| Azathioprine | Purine analog | Patients intolerant to CNIs | Cost-effective | Bone-marrow suppression |
| Belatacept | Costimulation blocker | Kidney transplant (long-term) | Zero nephrotoxicity | Higher early rejection, infusion-only |
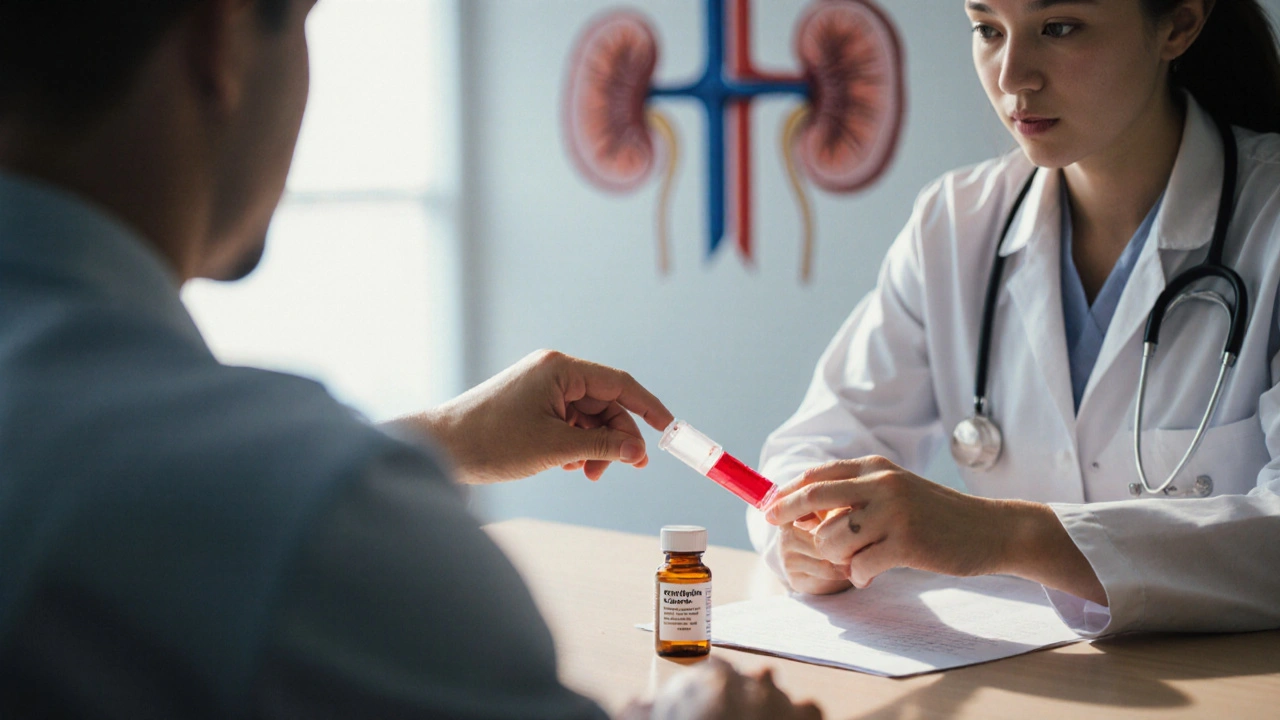
When you or a loved one need an immunosuppressant, the first name that pops up is often Cyclosporine (Imusporin), a drug that’s been a backbone of organ‑transplant regimens for decades. But cyclosporine isn’t the only game in town, and its side‑effect profile can be a deal‑breaker for many patients. This guide walks through the most common alternatives, weighs the pros and cons, and helps you figure out which option fits your health situation best.
Key Takeaways
- Cyclosporine remains highly effective for preventing organ rejection, but alternatives like tacrolimus and mycophenolate offer better kidney‑function safety for some patients.
- Choosing the right drug depends on the specific organ transplanted, co‑existing conditions, and how tolerant you are of monitoring requirements.
- Cost and insurance coverage vary widely; newer agents such as belatacept may be pricey but reduce long‑term nephrotoxicity.
- Drug‑interaction potential is a major factor - always review your full medication list before switching.
- Regular blood‑level checks are essential for most immunosuppressants, though the frequency differs by drug.
What Is Cyclosporine (Imusporin)?
Cyclosporine is a calcineurin inhibitor that blocks T‑cell activation, thereby preventing the immune system from attacking a transplanted organ. It’s administered orally or intravenously, with typical adult dosing ranging from 3‑5mg/kg per day, split into two doses. The drug reached the market in the early 1980s and quickly became the standard of care for kidney, liver, and heart transplants.
Key attributes of cyclosporine include:
- Mechanism: Inhibits calcineurin, reducing interleukin‑2 production.
- Therapeutic window: Narrow; blood levels must stay between 100‑400ng/mL depending on the organ.
- Common side effects: Nephrotoxicity, hypertension, gum hyperplasia, hirsutism, and tremor.
Because of its narrow window, patients need regular trough‑level testing, usually every 1‑2weeks during the first three months, then monthly as stability is achieved.
Major Alternatives to Cyclosporine
Below are the most frequently used substitutes, each with its own safety and efficacy profile.
Tacrolimus
Tacrolimus (brand names Prograf, Envarsus) is another calcineurin inhibitor but binds to a different intracellular protein, offering slightly higher potency. Typical adult dosing is 0.1‑0.2mg/kg per day, divided into twice‑daily doses. Many transplant centers prefer tacrolimus for kidney transplants because it’s associated with lower rates of chronic nephrotoxicity compared with cyclosporine.
Advantages include stronger rejection prophylaxis and fewer cosmetic side effects (no gum hyperplasia). However, tacrolimus can cause diabetes, neurotoxic symptoms, and the same need for blood‑level monitoring.
Sirolimus (Rapamycin)
Sirolimus works by inhibiting the mammalian target of rapamycin (mTOR) pathway, which blocks T‑cell proliferation without affecting calcineurin. Dosing usually starts at 2mg daily, aiming for trough levels of 5‑15ng/mL. Sirolimus is often added to a low‑dose calcineurin inhibitor to reduce nephrotoxicity.
Its side‑effect profile includes hyperlipidemia, delayed wound healing, and mouth ulcers. Because it doesn’t cause nephrotoxicity, sirolimus is a good option for patients with pre‑existing kidney issues.
Mycophenolate Mofetil (MMF)
Mycophenolate mofetil (CellCept) is an antimetabolite that blocks guanine nucleotide synthesis, thereby suppressing B‑ and T‑cell proliferation. Standard dosing is 1‑1.5g twice daily. MMF is rarely used alone for induction but is a cornerstone of maintenance regimens when paired with a calcineurin inhibitor.
Benefits include lower nephrotoxicity and less hypertension. The main drawbacks are gastrointestinal upset and an increased risk of infections, especially viral (CMV) reactivation.
Azathioprine
Azathioprine is a purine analog that interferes with DNA synthesis in rapidly dividing cells. Doses range from 1‑3mg/kg per day. It’s less potent than the newer agents, which means higher rejection rates when used alone, but it’s inexpensive and has a well‑characterized safety record.
Typical side effects are bone‑marrow suppression and liver enzyme elevation. Because of its lower potency, azathioprine is usually reserved for patients who cannot tolerate calcineurin inhibitors.
Belatacept
Belatacept is a fusion protein that blocks the CD80/86‑CD28 costimulatory pathway, preventing T‑cell activation. It’s given as an IV infusion (10mg/kg on days 0, 14, 30, then every 4weeks). Belatacept’s biggest selling point is its lack of nephrotoxicity, making it a compelling option for long‑term kidney‑transplant patients.
The trade‑off is higher early‑post‑transplant rejection rates and a higher cost compared with oral agents. It also requires regular infusion visits, which can be a logistical hurdle.
Side‑by‑Side Comparison
| Drug | Drug Class | Typical Indication | Primary Advantage | Major Drawback | Monitoring Requirement |
|---|---|---|---|---|---|
| Cyclosporine | Calcineurin inhibitor | Kidney, liver, heart transplant | Proven long‑term efficacy | Nephrotoxicity, cosmetic side effects | Trough level every 1‑2weeks |
| Tacrolimus | Calcineurin inhibitor | Kidney transplant (preferred) | Lower chronic kidney damage | Diabetes, neurotoxicity | Trough level every 1‑2weeks |
| Sirolimus | mTOR inhibitor | Adjunct to CNI, coronary‑artery stent patients | No nephrotoxicity | Delayed wound healing, hyperlipidemia | Trough level every month |
| Mycophenolate mofetil | Antimetabolite | Maintenance therapy with CNI | Low blood‑pressure impact | GI upset, infection risk | None (clinical labs only) |
| Azathioprine | Purine analog | Patients intolerant to CNIs | Cost‑effective | Bone‑marrow suppression | CBC every 2‑4weeks |
| Belatacept | Costimulation blocker | Kidney transplant (long‑term) | Zero nephrotoxicity | Higher early rejection, infusion‑only | Infusion schedule; labs for infection monitoring |
Decision Factors to Weigh
Choosing the best immunosuppressant isn’t a one‑size‑fits‑all decision. Here are the major levers you’ll likely discuss with your transplant team.
- Organ type and rejection risk - Kidney transplants have higher chronic‑nephrotoxicity concerns, pushing many surgeons toward tacrolimus or belatacept. Liver and heart grafts tolerate cyclosporine well.
- Pre‑existing health conditions - Diabetes or a history of hypertension makes tacrolimus less attractive, while prior kidney disease steers you away from cyclosporine.
- Side‑effect tolerance - If cosmetic changes (gum growth, hirsutism) bother you, tacrolimus and sirolimus are cleaner choices.
- Monitoring logistics - Frequent blood draws can be a burden; drugs like mycophenolate and azathioprine need far less level testing.
- Cost and insurance coverage - Generic cyclosporine and azathioprine are cheap, whereas belatacept can run several thousand dollars per year.
- Drug‑interaction profile - Cyclosporine and tacrolimus are metabolized by CYP3A4, so they clash with many antibiotics and antifungals. Sirolimus shares the same pathway, while mycophenolate has fewer interactions.

How to Choose the Right Regimen for You
Below is a quick‑reference guide that matches common patient scenarios with the most suitable drug class.
- New kidney transplant, no diabetes - Tacrolimus (plus MMF) is often first‑line.
- Kidney transplant + pre‑existing diabetes - Consider Sirolimus or belatacept to avoid worsening glucose control.
- Liver transplant, stable kidney function - Cyclosporine remains a solid choice.
- Patient cannot tolerate oral meds - Belatacept’s IV route can be a workaround, despite cost.
- Budget constraints - Azathioprine combined with low‑dose cyclosporine can keep expenses down while still offering protection.
Remember, the best plan is a partnership between you, your transplant surgeon, and your pharmacist. Keep notes on side effects, lab results, and how you feel day‑to‑day, then bring that data to each follow‑up.
Practical Tips & Common Pitfalls
- Never skip a trough‑level test. Even a small missed dose can swing the blood level into a dangerous range. \n
- Stay hydrated. Dehydration can increase cyclosporine concentration and raise kidney‑injury risk.
- Alert your doctor before starting over‑the‑counter meds like NSAIDs or herbal supplements; many interact with calcineurin inhibitors.
- Watch for early signs of infection (fever, cough, urinary symptoms) - immunosuppression masks typical fever spikes.
- If you notice new‑onset tremor, gum swelling, or unexplained high blood pressure, request a medication review immediately.
Frequently Asked Questions
Can I switch from cyclosporine to another drug after a transplant?
Yes, but only under close medical supervision. Switching usually involves a taper‑down period for cyclosporine while gradually introducing the new agent, with frequent blood‑level checks to avoid rejection.
Which alternative has the lowest risk of kidney damage?
Belatacept and sirolimus are the only agents that do not cause direct nephrotoxicity. For many patients, belatacept is the preferred choice when long‑term kidney health is a priority.
Do I need blood‑level monitoring for mycophenolate mofetil?
Routine therapeutic drug monitoring isn’t required for MMF, but labs are done to watch for anemia, liver‑enzyme changes, and infection markers.
Is tacrolimus more expensive than cyclosporine?
In most markets, generic tacrolimus costs a bit more than generic cyclosporine, but the price difference is usually modest. Insurance plans often cover both, so out‑of‑pocket costs vary by provider.
What should I do if I miss a dose of cyclosporine?
Take the missed dose as soon as you remember, unless it’s almost time for the next scheduled dose. In that case, skip the missed one and continue the regular schedule. Never double up.
Whether you stay on cyclosporine or switch to an alternative, the goal is the same: keep your transplanted organ thriving while maintaining a quality life. By understanding each drug’s strengths and weaknesses, you can have an informed conversation with your care team and make a choice that aligns with your health goals.



Hey folks! If you're diving into the world of immunosuppressants, think of it like picking the right paint for a masterpiece-each hue has its own vibe. Cyclosporine has been the classic splash, but there’s a whole palette out there. Let’s chat about how tacrolimus can keep kidneys happier, or how belatacept might just be the sleek, modern finish you never knew you needed. 🎨