Prostate Cancer Medication: What You Need to Know
When dealing with Prostate Cancer Medication, drugs specifically designed to treat or manage prostate cancer, ranging from hormone blockers to targeted therapies. Also known as PCa drugs, it plays a central role in modern oncology care. Prostate cancer medication is part of a broader treatment landscape that includes surgery, radiation, and active surveillance, and it often determines the course of long‑term disease control. Understanding what these meds do, how they are chosen, and what side‑effects to expect is the first step toward a plan that fits your lifestyle and health goals.
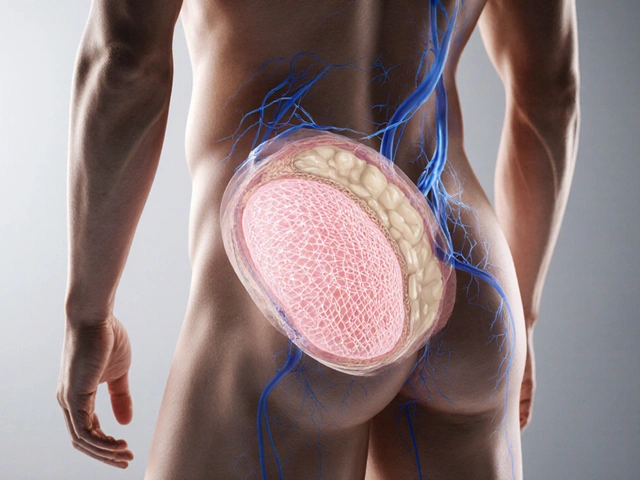
One major class is Androgen Deprivation Therapy (ADT), a hormone‑blocking regimen that lowers testosterone to slow tumor growth. ADT can be delivered as injections, implants, or oral agents, and it is usually the backbone of treatment for metastatic disease. It often pairs with Chemotherapy agents, drugs like docetaxel that attack rapidly dividing cancer cells when cancer becomes resistant to hormone suppression alone. For patients with advanced disease, Immunotherapy drugs, such as pembrolizumab that boost the immune system’s ability to recognize tumor cells are becoming a viable option, especially after genetic testing shows high microsatellite instability. These therapies intersect with Radiation therapy, targeted high‑energy beams used to shrink tumors before or after medication, creating a synergistic effect that can improve local control and reduce recurrence risk. In semantic terms: Prostate cancer medication encompasses ADT; ADT requires hormone monitoring; Immunotherapy influences tumor‑immune interaction; Radiation therapy supports medication efficacy; Chemotherapy agents target rapidly dividing cancer cells. Together, they form a network of choices that doctors balance based on PSA levels, imaging results, patient age, comorbidities, and personal preferences.
How These Treatments Fit Into Your Care Plan
Understanding the nuances of each drug class helps you and your doctor pick the right combo. ADT’s side‑effects—hot flashes, loss of bone density, fatigue, and metabolic changes—need regular bone scans and blood work, and many clinicians add bisphosphonates or denosumab to protect the skeleton. Chemotherapy requires careful dosing schedules, often every three weeks, and close monitoring of blood counts to prevent infection or anemia; supportive medications like growth‑factor injections can keep you on track. Immunotherapy may trigger immune‑related dermatitis, colitis, or thyroid issues, which are usually manageable with short courses of steroids if caught early. Radiation, whether external beam or brachytherapy, is planned around the timing of medication; for instance, delivering radiation after ADT can shrink the prostate and make the radiation field smaller, reducing damage to surrounding tissue. Cost also matters—generic ADT agents tend to be affordable, whereas newer immunotherapies can run into thousands of dollars per infusion, making insurance navigation a key part of the decision. Lifestyle tweaks such as strength training, a calcium‑rich diet, and stress‑reduction practices can lessen side‑effects and improve overall wellbeing.
By grasping how these pieces connect, you’ll spot the patterns that guide real‑world decisions—whether you’re looking at first‑line options, salvage therapy after a relapse, or enrollment in a clinical trial that tests a novel combination. The articles below break down specific drugs, compare benefits and risks, and share practical tips for navigating insurance, handling side‑effects, and making lifestyle adjustments that keep you in control of your health journey. Dive into the collection to find the information that matches your stage of treatment and personal priorities.
Flutamide (Eulexin) vs. Top Anti‑Androgen Alternatives - Quick Comparison
- Date: 20 Oct 2025
- Categories:
- Author: David Griffiths
Compare flutamide (Eulexin) with top anti‑androgen alternatives, covering efficacy, side‑effects, dosing, cost, and when to choose each option.