Obesity Treatment: What Actually Works and Why Most Diets Fail
When we talk about obesity treatment, a medical approach to managing excess body fat that addresses biological drivers, not just willpower. Also known as weight management therapy, it’s no longer just about calories in versus calories out—it’s about how your body’s hunger and energy systems have gone off track. The old idea that obesity is simply a lack of discipline? That’s outdated. Research shows it’s a complex disorder of appetite regulation, the biological system that tells you when to eat and when to stop and metabolic dysfunction, how your body burns or stores energy at a cellular level. People with obesity aren’t eating more because they’re weak—they’re eating more because their brain isn’t getting the right signals from hormones like leptin and ghrelin. Diets often fail because they don’t fix this broken system—they just starve it, which makes the body fight harder to regain weight.
That’s why newer obesity treatment approaches focus on biology, not willpower. Drugs like semaglutide and tirzepatide—GLP-1 agonists, medications that mimic a natural gut hormone to reduce hunger and slow digestion—aren’t magic pills. They’re tools that help reset the body’s broken appetite controls. These aren’t just for people who are "really" overweight—they work for anyone whose body has lost its natural ability to regulate food intake. And they’re not the only option. Lifestyle changes still matter, but they work better when paired with treatments that fix the underlying biology. Exercise helps, but it won’t override a hormone system that’s screaming for food. Sleep, stress, and even gut bacteria play roles too. This isn’t about willpower. It’s about science.
What you’ll find in the posts below isn’t a list of quick fixes. It’s a collection of real, evidence-based insights into how obesity treatment has changed. You’ll read about why diets backfire, how new medications actually work in the body, and why some people lose weight easily while others struggle despite doing everything "right." You’ll see how appetite regulation fails, what metabolic dysfunction really means, and how GLP-1 agonists are reshaping the field. There’s no fluff. No vague advice. Just clear, practical facts from the latest research—so you understand what’s happening in your body, and what options actually make a difference.
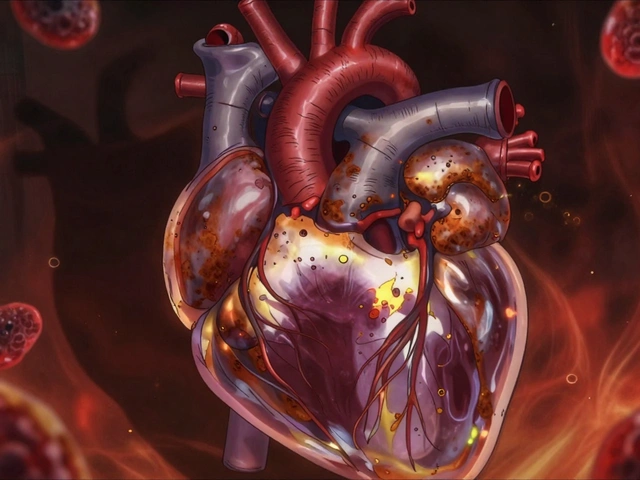
Obesity Comorbidities: How Diabetes, Heart Disease, and Sleep Apnea Connect and What to Do About It
- Date: 9 Dec 2025
- Categories:
- Author: David Griffiths
Obesity doesn't just affect weight-it triggers diabetes, heart disease, and sleep apnea in a dangerous cycle. Learn how these conditions connect, why treating them together matters, and what actually works to break the chain.