Drug Absorption: How Your Body Takes in Medications and Why It Matters
When you swallow a pill, it doesn’t just disappear and start working. Drug absorption, the process by which a medication enters your bloodstream from its site of administration. Also known as bioavailability, it determines how much of the drug actually reaches your system to do its job. A drug might be powerful on paper, but if your body can’t absorb it properly, it’s basically useless. This isn’t magic—it’s biology. And it’s the reason why some pills work better with food, why injections act faster than tablets, and why your doctor asks if you took your medicine on an empty stomach.
Bioavailability, the percentage of a drug that enters circulation unchanged is the key metric here. For example, if a drug has 80% bioavailability, 20% of it gets broken down before it ever reaches your blood. That’s why some drugs come in higher doses than others—they’re designed to compensate for poor absorption. Gastrointestinal tract, the path from mouth to colon where most oral drugs are absorbed plays a huge role. Stomach acid, gut bacteria, and even the lining of your intestines can make or break how well a drug gets in. Some medications, like certain antibiotics or GLP-1 agonists, are designed to survive stomach acid so they can be absorbed in the small intestine. Others, like nitroglycerin, are given under the tongue because the mouth absorbs them faster than the gut ever could.
It’s not just about where the drug goes—it’s about when. Eating a big meal can delay absorption, sometimes by hours. That’s why some meds say "take on an empty stomach." On the flip side, fat-soluble drugs like some cholesterol meds work better when taken with food. Even your age, gut health, or other medications you’re taking can interfere. For instance, antacids can block absorption of certain antibiotics, and iron supplements can mess with thyroid meds. Pharmacokinetics, the study of how your body moves drugs through absorption, distribution, metabolism, and excretion explains why timing matters so much. A drug taken at the wrong time might not just be less effective—it could cause side effects or even become toxic.
What you’ll find in the posts below isn’t just a list of drugs. It’s a practical guide to how real medications behave in real bodies. You’ll see how isotretinoin needs fat to absorb properly, why some antibiotics work better on an empty stomach, and how EHR systems help pharmacists catch absorption issues before they cause harm. You’ll learn how drug interactions—like steroids with NSAIDs—can change how your body handles meds. And you’ll get clear, no-nonsense advice on how to make sure your pills actually work the way they’re supposed to.
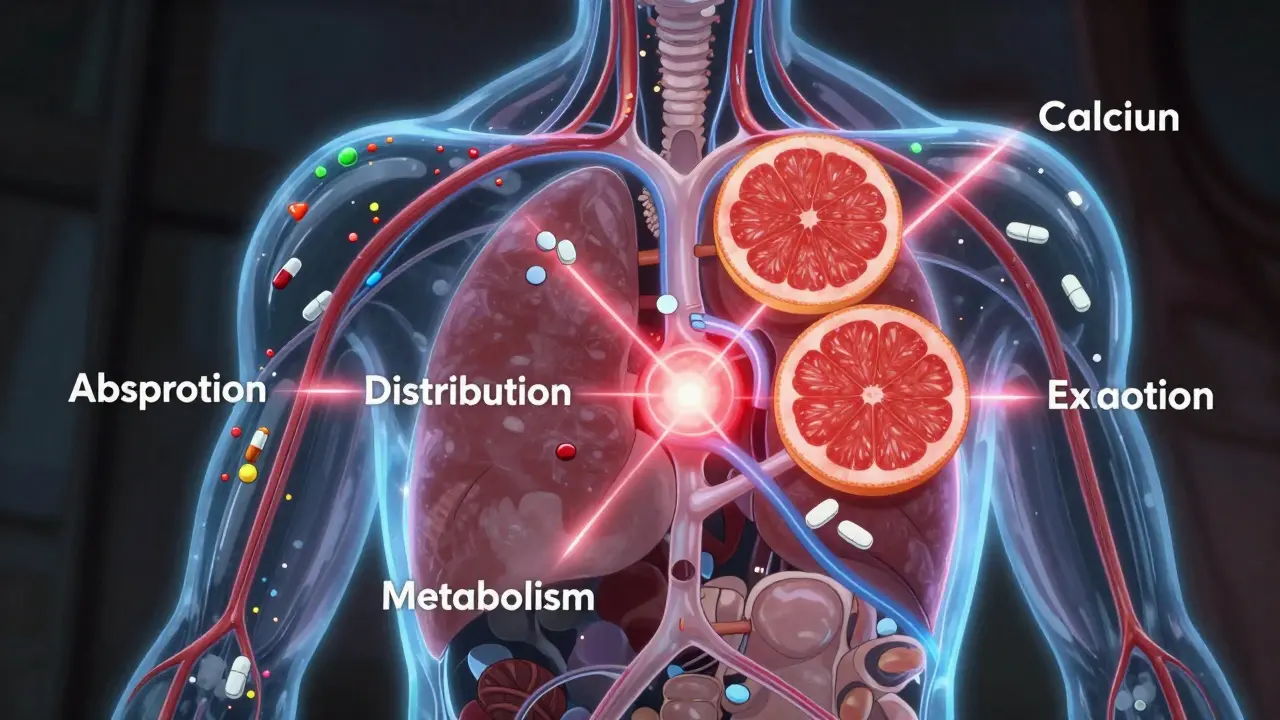
Pharmacokinetic Drug Interactions Explained for Patients: What You Need to Know
- Date: 22 Jan 2026
- Categories:
- Author: David Griffiths
Learn how one medication can change how your body processes another-through absorption, metabolism, or excretion. Simple steps to avoid dangerous drug interactions and stay safe.
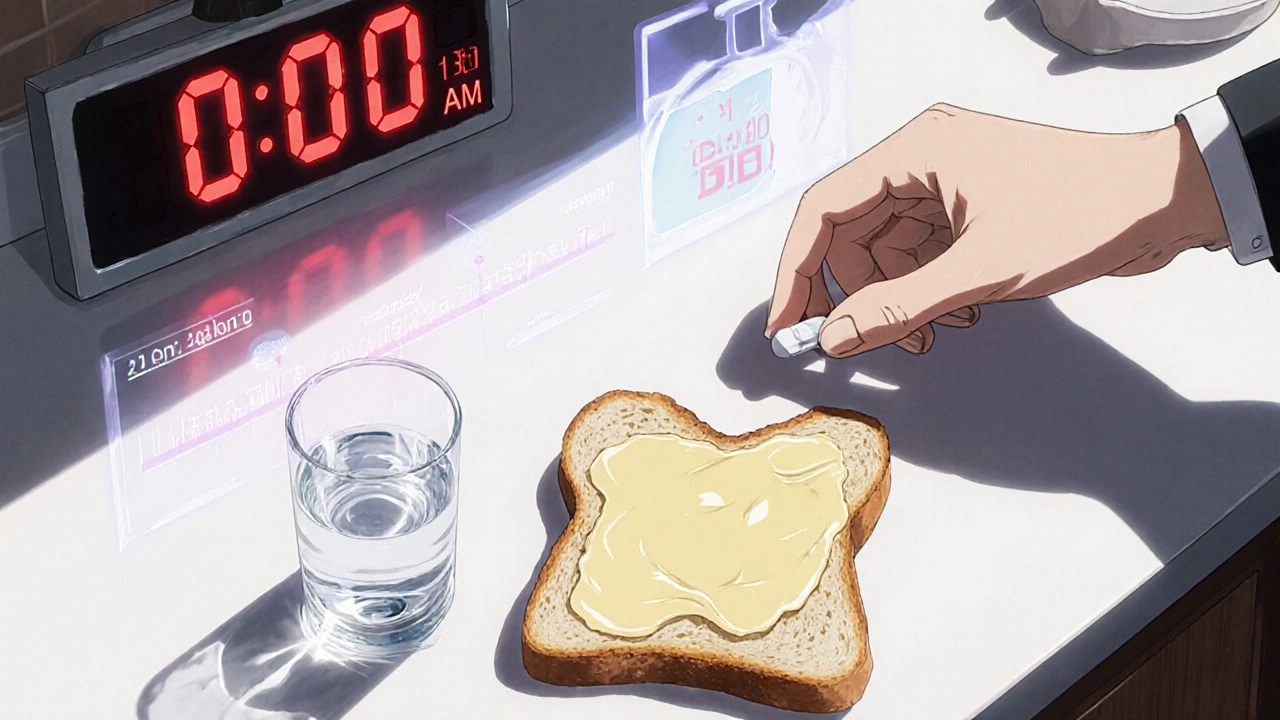
Taking Medications with Food: How Meals Affect Absorption and Timing
- Date: 18 Nov 2025
- Categories:
- Author: David Griffiths
Learn how food affects medication absorption and timing. Discover which drugs need an empty stomach, which need food, and why getting it wrong can reduce effectiveness or cause side effects.