Have you ever taken a new pill and suddenly felt off? Maybe you got dizzy after starting a new antibiotic, or your blood thinner seemed to work too well after eating grapefruit. These aren’t just bad luck-they could be pharmacokinetic drug interactions. This isn’t about drugs fighting each other in your body. It’s about how one drug changes how your body handles another-how it’s absorbed, distributed, broken down, or flushed out. And when that happens, things can go wrong fast.
How Your Body Moves Drugs Around
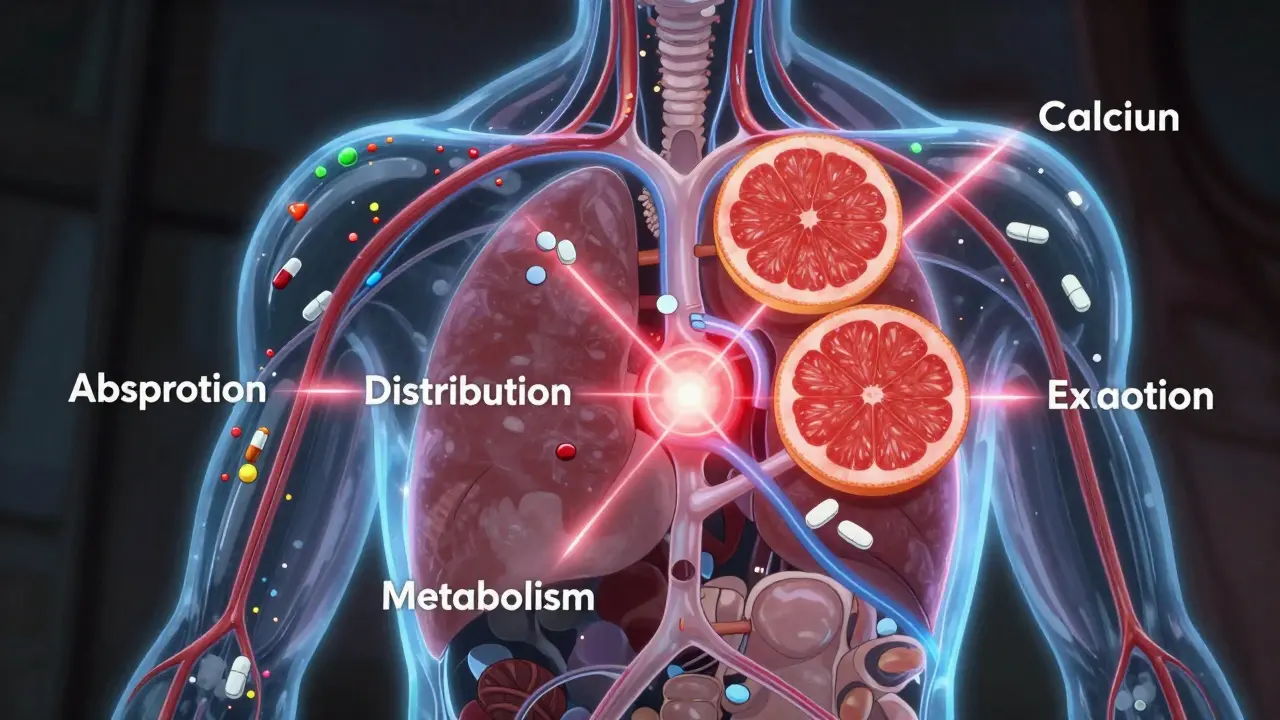
Think of your body like a delivery system. Every drug you take needs to get to the right place at the right time. That process is called pharmacokinetics-your body’s four-step journey for a drug: Absorption, Distribution, Metabolism, and Excretion. Doctors call this ADME. If one drug messes with any of those steps, the amount of the other drug in your blood can go too high or too low. Too high? You might overdose. Too low? The drug stops working.Absorption: When Your Stomach Says No
Not all drugs get absorbed the same way. Some need an acidic stomach to work. Others get blocked by food or other meds. For example, the antibiotic tetracycline binds to calcium in milk, yogurt, or antacids. That binding stops it from being absorbed. Studies show this can cut its effectiveness by up to 50%. The fix? Take tetracycline at least 2-3 hours before or after dairy or calcium supplements. Another common problem is with ketoconazole, an antifungal. It needs stomach acid to dissolve properly. If you take an antacid or proton pump inhibitor (like omeprazole) at the same time, ketoconazole won’t absorb well. You might think the treatment isn’t working-but it’s just stuck in your gut. Even something as simple as acetaminophen (Tylenol) can be delayed by opioids like morphine. These slow down your stomach and intestines, pushing the painkiller’s absorption later than expected. It’s not dangerous, but it means you won’t feel relief when you expect it.Distribution: The Protein Swap Game
Once a drug gets into your bloodstream, it sticks to proteins-mostly albumin-to travel around. But there’s only so much room. When two drugs fight for the same spot, one can get pushed off. That’s called displacement. The classic example is warfarin (a blood thinner) and diclofenac (an NSAID painkiller). Diclofenac kicks warfarin off its protein binding, leaving more free warfarin in your blood. Since only the free part works, your blood thinning effect spikes. That raises your risk of serious bleeding-even if your usual warfarin dose hasn’t changed. But here’s the catch: this doesn’t happen often. Your body usually adjusts by breaking down the extra free drug faster. So unless the drug has a very narrow safety window-like warfarin, digoxin, or phenytoin-it’s usually not a big deal. Still, if you’re on one of these high-risk meds, your doctor needs to know everything you’re taking.
Metabolism: The Liver’s Hidden Boss
This is where the most dangerous interactions happen. About 80% of drugs are broken down by enzymes in your liver-especially the cytochrome P450 system. Think of these enzymes like tiny scissors that chop up drugs so your body can get rid of them. Sometimes, one drug acts like a blocker. It jams the scissors. That means another drug builds up in your blood. For example:- Grapefruit juice blocks CYP3A4, a major enzyme. That can cause dangerous spikes in drugs like simvastatin (a statin), felodipine (a blood pressure med), or midazolam (a sedative). One grapefruit can affect you for 24 hours.
- Clarithromycin (an antibiotic) and fluoxetine (an antidepressant) also block CYP3A4 and CYP2D6. If you’re taking metoprolol (a beta-blocker), your dose may need to be cut in half.
- St. John’s Wort (a supplement for mild depression) speeds up CYP3A4 and CYP2D6. It can make birth control pills, antidepressants, and even HIV meds stop working.
- Rifampin (used for tuberculosis) and carbamazepine (for seizures) do the same thing. One patient on lamotrigine (for epilepsy) developed dangerous blood cell drops because rifampin pushed lamotrigine into toxic metabolites.
Excretion: The Kidney’s Final Checkpoint
Your kidneys are the last stop. They flush drugs out through urine. But if two drugs use the same exit route, they can block each other. For example, probenecid (used for gout) blocks the kidney’s ability to clear cephalosporin antibiotics. That raises antibiotic levels-and increases your risk of side effects. Even more dangerous is the interaction between NSAIDs (like ibuprofen or naproxen) and methotrexate (used for arthritis and cancer). NSAIDs can stop methotrexate from leaving your body, leading to bone marrow damage or kidney failure. There’s also P-glycoprotein, a transporter that kicks drugs out of your kidney and gut cells. If a drug like itraconazole (an antifungal) blocks it, digoxin (for heart rhythm) builds up. That can cause life-threatening irregular heartbeats. The FDA says about 20% of serious drug interactions involve these transporter systems. Digoxin, warfarin, and immunosuppressants like cyclosporine are especially risky.Real-Life Consequences
These aren’t just theory. A real case involved an 85-year-old woman on venlafaxine (an antidepressant) and propafenone (a heart rhythm drug). Both are processed by CYP2D6 and blocked by P-gp. Together, venlafaxine levels soared. She developed hallucinations and agitation. Her meds were stopped-and she recovered. Another patient on phenobarbital (for seizures) and lamotrigine developed dangerously low white blood cell counts. The phenobarbital had triggered toxic metabolites of lamotrigine. This is why doctors monitor blood counts closely when combining these drugs. The Institute for Safe Medication Practices says warfarin, insulin, and digoxin are the top three drugs involved in interaction-related ER visits. Together, they account for one-third of all serious cases.
How to Protect Yourself
You don’t have to memorize enzyme names or drug mechanisms. But you can take simple steps that cut your risk dramatically:- Keep a full list of everything you take: prescriptions, over-the-counter pills, vitamins, herbs, and supplements. A 2020 study found this reduces interaction risks by 47%.
- Use one pharmacy. Pharmacies scan all your meds and flag conflicts. In the U.S., this prevents about 150,000 adverse events every year.
- Ask these two questions every time you get a new prescription: “Could this interact with my other meds?” and “Are there foods or drinks I should avoid?” Mayo Clinic research shows this increases detection by 63%.
- Avoid grapefruit juice if you’re on any of the 85+ drugs known to interact with it. That includes statins, blood pressure meds, and some anti-anxiety drugs.
- Space out tricky combos. If you take thyroid medicine (like levothyroxine), wait at least 4 hours before taking calcium, iron, or antacids. They block absorption.
What Your Doctor and Pharmacist Are Doing
Your healthcare team isn’t just guessing. Electronic health records now have built-in alerts that catch 85% of major interactions. But doctors get so many alerts-many of them low-risk-that they ignore nearly half. That’s why your pharmacist’s role is more important than ever. Pharmacists run medication reviews that cut adverse events by 22% in older adults. Tools like Lexicomp, Micromedex, and Stockley’s Drug Interactions give them real-time data on mechanisms and solutions. In the U.S., pharmacist-led reviews prevent 1.2 million serious interactions every year. The future? Personalized medicine. The FDA now includes pharmacogenomic info on 340 drug labels. That means your genes can tell your doctor if you’re a slow or fast metabolizer. For example, if you’re a CYP2C19 poor metabolizer, you might need a different dose of clopidogrel (a heart drug). This could reduce interaction-related hospitalizations by up to 30%.Bottom Line
Pharmacokinetic drug interactions are invisible-but they’re real. They don’t always cause symptoms right away. But when they do, the results can be life-changing-or life-ending. You don’t need to be a scientist to stay safe. Just be your own advocate. Keep your list updated. Talk to your pharmacist. Ask the two simple questions. And never assume a supplement is harmless just because it’s natural. St. John’s Wort isn’t tea-it’s a powerful enzyme inducer. Your body is a complex system. Medications are powerful tools. When used right, they heal. When mixed wrong, they harm. Stay informed. Stay alert. And never stop asking questions.What’s the difference between pharmacokinetic and pharmacodynamic drug interactions?
Pharmacokinetic interactions are about how your body moves a drug-absorption, distribution, metabolism, or excretion. Pharmacodynamic interactions are about how drugs affect your body together. For example, taking two drugs that both lower blood pressure can cause your pressure to drop too far-that’s pharmacodynamic. One drug slowing the breakdown of another is pharmacokinetic.
Can over-the-counter drugs cause serious interactions?
Absolutely. NSAIDs like ibuprofen and naproxen can raise your risk of bleeding if you’re on warfarin. Antacids can block antibiotics like tetracycline. Even common cold medicines with pseudoephedrine can spike your blood pressure if you’re on certain heart meds. Always check with your pharmacist before taking OTC drugs, especially if you’re on multiple prescriptions.
Is grapefruit juice really that dangerous with medications?
Yes. Grapefruit juice blocks the CYP3A4 enzyme in your gut, which breaks down over 85 prescription drugs. Even one glass can last 24 hours. It can cause dangerous spikes in statins (like simvastatin), blood pressure drugs (like felodipine), and sedatives (like midazolam). If your medication label says “avoid grapefruit,” don’t risk it. Orange juice is usually safe.
Why do some drug interactions only happen in older adults?
As we age, our liver and kidneys don’t work as well. About 40% of adults over 65 have reduced kidney function. That means drugs stick around longer. Also, older adults often take 5-10 medications at once, increasing chances of overlap. The American Geriatrics Society Beers Criteria lists high-risk drugs for seniors because their bodies handle them differently.
Should I stop taking a medication if I think it’s interacting?
Never stop a prescription medication on your own. Some drugs, like blood pressure or seizure meds, can cause serious withdrawal effects. Instead, call your doctor or pharmacist. They can tell you if it’s a real interaction, how serious it is, and what to do next-whether that’s adjusting the dose, spacing out times, or switching to a safer option.

I took grapefruit juice with my statin and woke up feeling like my muscles were turning to jelly. ER visit. ICU. $22k bill. Now I drink orange juice like it’s my job. 🍊💀