Diabetes Drug Alternatives
When navigating diabetes drug alternatives, medications that can replace or complement traditional insulin or sulfonylureas for managing blood sugar. Also known as alternative glucose‑lowering therapies, they offer varied mechanisms, costs, and side‑effect profiles. Understanding these options helps you balance effectiveness with price, especially if insurance coverage is tight.
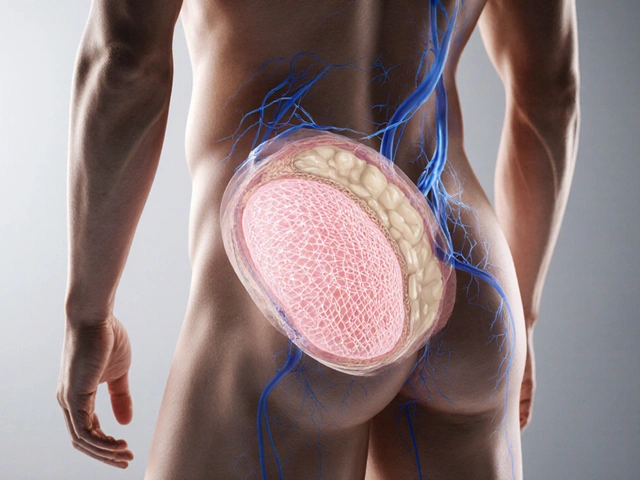
One of the most common alternatives is Glipizide, a first‑generation sulfonylurea that stimulates the pancreas to release more insulin. It’s cheap, widely available, and works well for many people with early‑stage type 2 diabetes. However, newer classes like SGLT2 inhibitors, drugs that force the kidneys to excrete excess glucose through urine provide added heart‑protective benefits and lower risk of low blood sugar. Choosing between them depends on your health goals, kidney function, and budget.
Another major player is the GLP‑1 agonist family. These injectables mimic a gut hormone that boosts insulin after meals, slows gastric emptying, and often leads to weight loss. Compared with older pills, they can improve cardiovascular outcomes but usually cost more. When cost matters, many patients combine a low‑dose GLP‑1 with a cheap sulfonylurea or metformin to get the best of both worlds. This hybrid approach illustrates the semantic link: diabetes drug alternatives require balancing efficacy, side‑effects, and affordability.
Key Factors to Evaluate When Picking an Alternative
First, look at the drug’s mechanism of action. Does it increase insulin release, improve insulin sensitivity, or reduce glucose reabsorption? Knowing the mechanism helps you avoid duplication and anticipate side‑effects. Second, check insurance formularies. Many plans favor generic sulfonylureas and metformin, while brand‑name SGLT2 or GLP‑1 agents may need prior authorization. Third, consider your comorbidities. If you have heart disease, an SGLT2 inhibitor might be a smarter pick than a cheap sulfonylurea. Finally, factor in administration convenience: oral pills are easier for most, but an injectable GLP‑1 could be worth the extra step if weight loss is a priority.
Cost‑saving strategies also play a big role. Stacking coupons, using 90‑day supplies, or opting for therapeutic equivalents can shave hundreds of dollars off a year’s expense. For example, a patient switching from brand‑name Glipizide to a reputable generic can save up to 60 % without losing potency. Similarly, many pharmacy discount programs list SGLT2 inhibitors at a lower price than the MSRP, especially when you combine them with a cheap sulfonylurea.
Real‑world experience shows that many people start with metformin, add a low‑cost sulfonylurea like Glipizide, and only move to newer agents if blood sugar remains uncontrolled. This stepwise approach mirrors the semantic triple: Diabetes drug alternatives encompass a progression from basic to advanced therapies. It also aligns with clinical guidelines that recommend escalating treatment only when necessary, keeping costs manageable.
Below you’ll find a curated collection of articles that dig deeper into each category—cost comparisons, side‑effect profiles, insurance tips, and patient stories. Whether you’re looking for a cheap oral option or a cutting‑edge injectable, the posts ahead break down the pros and cons so you can make an informed choice.
Empagliflozin vs Other Diabetes Drugs: Benefits, Risks & Alternatives
- Date: 26 Sep 2025
- Categories:
- Author: David Griffiths
An in‑depth look at empagliflozin, how it stacks up against other diabetes medicines, its heart‑protective effects, safety profile, and when to choose it.