Diabetes Medication Comparison Tool
Compare Diabetes Medications
Select two medications to compare their benefits and risks:
Empagliflozin is a selective sodium‑glucose co‑transporter‑2 (SGLT2) inhibitor approved for managing type 2 diabetes, reducing cardiovascular mortality, and slowing chronic kidney disease progression.
Why Empagliflozin matters for people with type 2 diabetes
When you hear "SGLT2 inhibitor," picture a drug that helps kidneys flush out excess glucose through urine. That simple mechanism translates into lower blood sugar, modest weight loss, and, crucially, a drop in heart‑failure hospitalisations. Empagliflozin hit the headlines after the EMPA‑REG OUTCOME trial showed a 38% reduction in cardiovascular death compared with placebo - numbers that still turn heads in 2025.
How it works: the SGLT2 pathway
The kidneys reabsorb about 180g of glucose every day via the SGLT2 protein in the proximal tubule. Empagliflozin blocks that transporter, causing 50‑70g of glucose to be excreted daily. The loss of calories nudges weight down by 2‑3kg on average, while the osmotic diuresis eases blood‑pressure control.
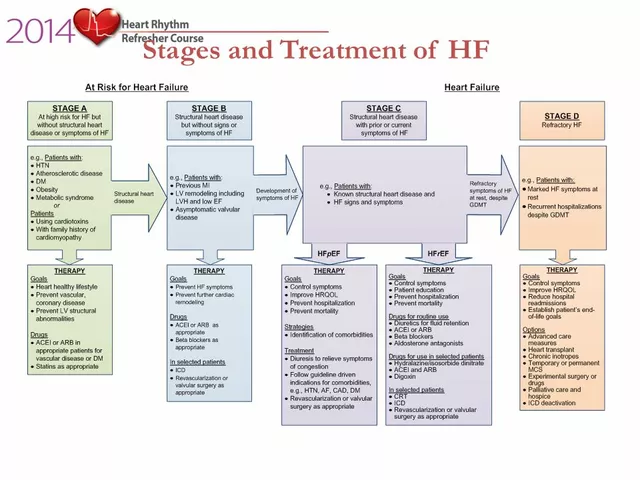
Key clinical outcomes
Beyond glucose control (average HbA1c drop of 0.6‑0.8%), three hard‑endpoint benefits dominate the conversation:
- Cardiovascular mortality: 38% lower risk in high‑risk patients (EMPA‑REG).
- Heart‑failure hospitalisation: 35% reduction, seen across broader populations in the EMPEROR‑Preserved and EMPEROR‑Reduced trials.
- Renal protection: 46% slower decline in eGFR and 55% lower risk of end‑stage kidney disease.
These outcomes earned empagliflozin a ClassI recommendation from the American Diabetes Association (ADA) for patients with established atherosclerotic cardiovascular disease.
Other SGLT2 inhibitors on the market
Empagliflozin isn’t the only player in the SGLT2 space. Two close cousins dominate the shelf:
Canagliflozin is a SGLT2 inhibitor launched in 2013, notable for its modest weight‑loss effect and a slightly higher dose range (100‑300mg). It earned a cardiovascular benefit label after the CANVAS program, showing a 14% reduction in major adverse cardiovascular events (MACE).
Dapagliflozin entered the market in 2014, with a once‑daily 10‑mg dose. The DECLARE‑TIMI 58 trial highlighted a 17% cut in cardiovascular death or hospitalisation for heart failure.
All three share the core glucose‑lowering action, but their trial data differ slightly in the magnitude of heart‑failure benefit and renal outcomes. Empagliflozin consistently tops the cardiovascular mortality charts, while dapagliflozin edges ahead on heart‑failure outcomes in patients without established atherosclerotic disease.
How Empagliflozin stacks up against non‑SGLT2 drugs
Two other drug classes dominate first‑line therapy:
Metformin is a biguanide that reduces hepatic glucose production; it's cheap, weight‑neutral, and carries a long safety record. Its cardiovascular impact is modest, with a 9% MACE reduction in the UKPDS follow‑up.
Semaglutide is a GLP‑1 receptor agonist that mimics the gut hormone GLP‑1, boosting insulin secretion, slowing gastric emptying, and promoting satiety. In the SUSTAIN‑6 trial, semaglutide cut major cardiovascular events by 26% and induced an average 4‑kg weight loss.
When you compare empagliflozin to these, the biggest differences are:
- Empagliflozin provides clear renal protection, which metformin lacks.
- Semaglutide offers stronger weight loss but requires injection (or oral version with lower bioavailability).
- Cost‑wise, metformin remains the cheapest; empagliflozin sits in the mid‑range, while GLP‑1 agents are usually pricier.

Safety profile and common side‑effects
Every medication has trade‑offs. Empagliflozin’s safety highlights include:
- Genital mycotic infections: Occur in 5‑10% of women and 2‑3% of men - often mild and treatable.
- Euglycaemic ketoacidosis: Rare (<0.1%) but serious; risk rises with low‑carb diets and insulin deficiency.
- Volume depletion: May cause dizziness, especially in the elderly or when combined with diuretics.
Canagliflozin carries a slightly higher amputation signal (particularly toe amputations), a risk not observed with empagliflozin. Dapagliflozin’s safety profile mirrors empagliflozin’s, but long‑term real‑world data suggest similar genital infection rates.
Practical decision guide: when to pick Empagliflozin
Imagine you’re a GP reviewing a 58‑year‑old man with HbA1c 8.2%, established coronary artery disease, and stage3 chronic kidney disease (eGFR 45mL/min/1.73m²). The choices are:
- Intensify metformin (already at max dose) - limited renal benefit.
- Add a GLP‑1 agonist - potent weight loss but injectable and costlier.
- Start empagliflozin - adds cardiovascular mortality reduction, slows kidney decline, and is oral.
Guidelines (ADA 2024) would rank empagliflozin as the preferred add‑on for this profile. In contrast, a younger patient with mild hyperglycaemia, no cardiovascular disease, and a strong preference for low‑cost pills might stay on metformin alone.
Related concepts and broader context
Understanding empagliflozin’s place involves a few surrounding ideas:
- Regulatory status: Approved by the FDA (2014), EMA, and Therapeutic Goods Administration (TGA) in Australia.
- Guideline evolution: The 2023 ADA/EASD consensus placed SGLT2 inhibitors ahead of basal insulin for patients with heart‑failure risk.
- Cost considerations: In Australia, the PBS lists empagliflozin with a co‑payment of about AU$30 per month, making it affordable for most retirees.
- Insurance coverage: Private insurers increasingly require prior‑authorization only for doses above 10mg.
- Future directions: Ongoing trials are testing empagliflozin in non‑diabetic heart‑failure populations, hinting at an even broader therapeutic role.
Quick comparison table
| Drug | Class | HbA1c reduction | Cardiovascular benefit | Renal benefit | Common side‑effects |
|---|---|---|---|---|---|
| Empagliflozin | SGLT2 inhibitor | 0.6‑0.8% | 38% ↓ CV death (EMPA‑REG) | 46% ↓ eGFR decline | Genital infections, volume depletion |
| Canagliflozin | SGLT2 inhibitor | 0.5‑0.7% | 14% ↓ MACE (CANVAS) | 30% ↓ renal endpoint | Amputations, genital infections |
| Dapagliflozin | SGLT2 inhibitor | 0.5‑0.7% | 17% ↓ CV death/HF (DECLARE) | 37% ↓ renal endpoint | Genital infections, UTIs |
| Metformin | Biguanide | 1.0‑1.5% | 9% ↓ MACE (UKPDS) | None proven | GI upset, lactic acidosis (rare) |
| Semaglutide | GLP‑1 RA | 1.2‑1.5% | 26% ↓ MACE (SUSTAIN‑6) | Modest renal benefit | Nausea, vomiting, pancreatitis risk |
Bottom line: is Empagliflozin the right choice?
If you or a loved one is grappling with type2 diabetes *and* carry any of the following, empagliflozin often makes the most sense:
- Established atherosclerotic cardiovascular disease.
- Evidence of early chronic kidney disease.
- History of heart‑failure hospitalisation.
- Desire for an oral regimen rather than injections.
For patients solely focused on modest glucose reduction without cardiovascular or renal concerns, metformin remains a solid first‑line option. When weight loss is a top priority and injection isn’t a barrier, GLP‑1 agents may be preferable.
Frequently Asked Questions
What makes empagliflozin different from other SGLT2 inhibitors?
Empagliflozin showed the strongest reduction in cardiovascular death in the EMPA‑REG trial, whereas canagliflozin and dapagliflozin have more modest MACE benefits. Its renal protection data are also slightly more robust, making it the preferred SGLT2 agent for patients with both heart and kidney risk.
Can I take empagliflozin if my eGFR is below 30?
Current labeling permits empagliflozin down to an eGFR of 20mL/min/1.73m², but efficacy diminishes as kidney function falls. For eGFR <30, many clinicians switch to a GLP‑1 agonist or adjust dosage while monitoring for side‑effects.
Do I need to worry about ketoacidosis on empagliflozin?
Euglycaemic ketoacidosis is rare but can happen, especially if you follow a very low‑carb diet or have reduced insulin. Staying hydrated, monitoring ketones when ill, and informing your doctor of any dietary changes can mitigate the risk.
How does empagliflozin compare cost‑wise to metformin or GLP‑1 drugs?
In Australia, empagliflozin is subsidised under the PBS with a co‑payment of about AU$30 per month, while metformin is essentially free on the PBS. GLP‑1 agents like semaglutide are priced higher, often exceeding AU$150 per month without additional subsidies.
Is empagliflozin safe for older adults?
Older patients benefit from the heart‑failure protection, but they are also more prone to volume depletion and orthostatic hypotension. Starting at the low 10mg dose, reviewing diuretic use, and checking kidney function regularly are key steps.



Hey everyone, I totally get the worry when you see numbers like a 38% cut in CV death-it can feel overwhelming. But empagliflozin's data are backed by solid trials, so it isnt just hype. If u have kidney issues, the drug actually slows eGFR decline, which is a huge plus. Side‑effects like yeast infections are real, but most folks manage them with simple hygiene tweaks. Bottom line, talk to ur doc and weigh the heart benefits against the modest weight loss.