Amgen v. Sanofi: Biotech Patent Battles and the Future of Cholesterol Drugs
When you hear Amgen v. Sanofi, a landmark legal dispute between two major pharmaceutical companies over patent rights to PCSK9 inhibitor drugs. Also known as the PCSK9 patent war, it’s not just about legal paperwork—it’s about who gets to control life-saving cholesterol treatments and how much patients pay for them. This wasn’t a minor disagreement. It was a five-year court battle that reached the U.S. Supreme Court, centered on whether Sanofi’s drug, Praluent, copied Amgen’s patented technology for blocking PCSK9, a protein that raises LDL (bad) cholesterol. The outcome didn’t just affect two companies—it reshaped how biotech patents are written, enforced, and challenged.
At the heart of this fight were PCSK9 inhibitors, a new class of injectable drugs designed to lower cholesterol far beyond what statins can do. These drugs, including Amgen’s Repatha and Sanofi’s Praluent, work by disabling PCSK9, letting the liver remove more bad cholesterol from the blood. Unlike pills, they’re injected monthly and can cut LDL levels by 50% or more. But they’re expensive—often over $14,000 a year—so insurers and patients needed proof they were truly different from existing treatments. That’s where the patent claims came in: Amgen argued Sanofi stole its discovery, while Sanofi said they built something new using public science.
The Supreme Court’s 2023 decision sided with Amgen, saying its patent was too broad and didn’t clearly define what made its invention unique. That ruling sent shockwaves through the biotech world. It meant companies can’t just patent a general idea—like "blocking PCSK9 to lower cholesterol"—and stop others from making any version of it. Now, patent holders must spell out exact molecular structures, not broad functions. This change helps smaller drugmakers enter the market, lowers prices, and speeds up innovation. It also explains why newer PCSK9 alternatives, like inclisiran (Leqvio), are now available with fewer restrictions.
Meanwhile, the battle over drug competition, the push to bring more affordable versions of high-cost medicines to patients. Also known as biosimilar competition, it’s why you now see generic versions of biologics slowly appearing after patents expire. The Amgen v. Sanofi case didn’t just decide who owned a patent—it set a new standard for how future drug patents will be written, making it harder to block rivals with vague claims.
What does this mean for you? If you or someone you know takes a PCSK9 inhibitor, you’re seeing the direct result of this legal fight. Lower prices, more choices, and faster access to better treatments are all outcomes of this battle. The same rules now apply to cancer drugs, autoimmune therapies, and other biologics. This isn’t just corporate drama—it’s about whether life-changing medicines stay locked behind legal walls or become widely available.
Below, you’ll find real-world guides on how these drugs work, how they compare to other treatments, and how to manage side effects—backed by patient experiences and clinical data. Whether you’re managing high cholesterol, navigating insurance approvals, or just trying to understand why your prescription costs what it does, these posts cut through the noise and give you what matters.
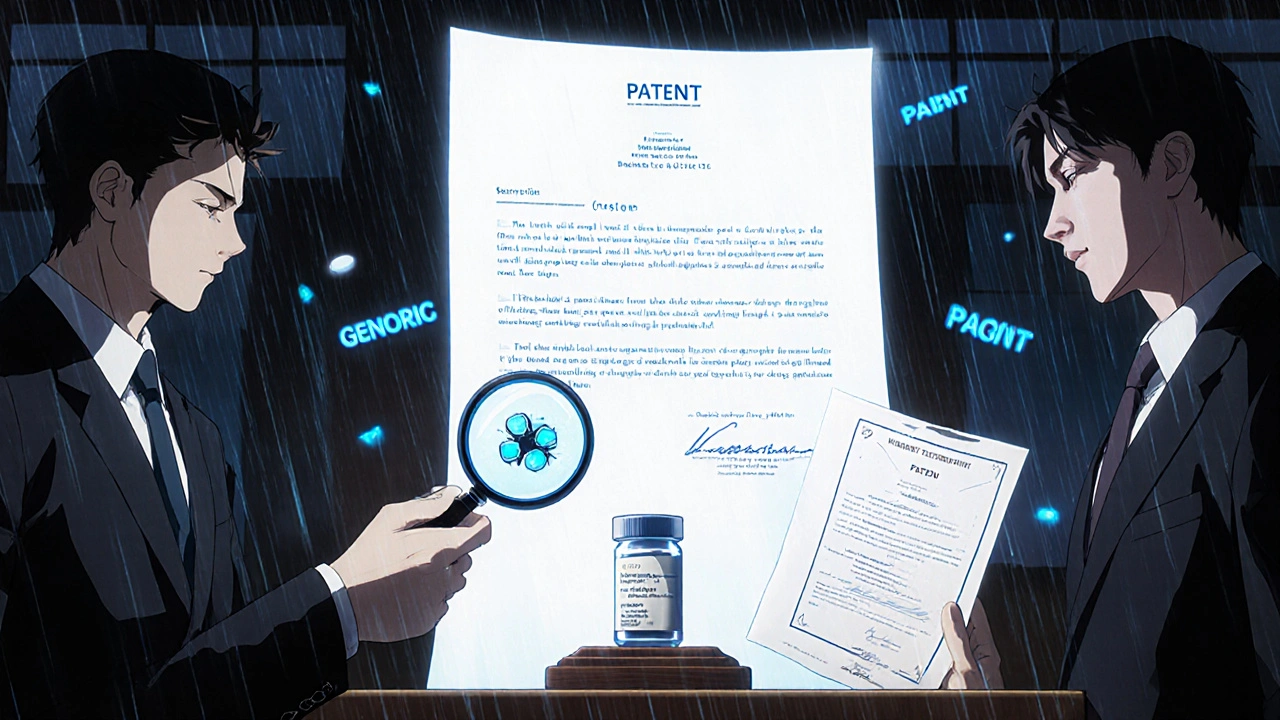
Generic Patent Case Law: Landmark Court Decisions That Shape Drug Prices
- Date: 22 Nov 2025
- Categories:
- Author: David Griffiths
Landmark court decisions like Amgen v. Sanofi and Allergan v. Teva are reshaping how generic drugs enter the market, directly impacting drug prices and patient access. Learn how patent law, the Orange Book, and IPRs determine when generics become available.