Anesthesia Recovery Tracker
Recovery Phase Tracker
Recovery Timeline
Your Recovery Status
Coming home from the operating theatre feels like a win, but the first 24‑48 hours can be a roller‑coaster if you’re not prepared. Knowing what to expect from Anesthesia recovery - the period when your body wakes up from the drugs that kept you asleep - can cut anxiety, speed healing, and keep complications at bay.
What Exactly Is Anesthesia Recovery?
Anesthesia recovery is the phase after the anesthetic agents wear off and you transition from a medically induced unconscious state back to normal consciousness. It starts the moment the surgeon closes the wound and continues until you’ve regained baseline mental clarity, stable vital signs, and can safely perform basic activities like walking and drinking fluids.
Typical Timeline - How Long Does It Take?
- 0-30 minutes: You’re in the post‑anesthesia care unit (PACU). Drowsiness, a metallic taste, and mild nausea are common.
- 30‑120 minutes: Vital signs stabilize, pain spikes, and you may experience grogginess or “brain fog.”
- 2‑4 hours: Most patients can sit up, sip water, and may be discharged if criteria are met.
- Day 1‑2: Residual drowsiness fades, but sore throat (from the airway tube), muscle aches, and occasional itching from opioids persist.
- Day 3‑7: Cognitive function typically returns to baseline; any lingering nausea or constipation should improve.
These are averages. Individual timelines shift based on age, type of surgery, and the anesthetic used.
Why Realistic Expectations Matter
When you picture a smooth wake‑up, you’re often imagining a Hollywood recovery-instant alertness, zero pain, and a quick return to normal life. The reality is messier, and that mismatch can have real consequences:
- Reduced anxiety: Knowing that a foggy head for a few hours is normal calms nerves.
- Improved compliance: You’re more likely to follow pain‑medication schedules and hydration advice if you understand why they matter.
- Lowered risk of complications: Recognising a normal side‑effect versus a warning sign (like uncontrolled bleeding) prevents delayed medical attention.
Common Misconceptions and the Truth Behind Them
| Myth | Fact |
|---|---|
| I’ll be fully awake within minutes. | Most people feel groggy for 1‑2 hours; brain function normalises over 24‑48 hours. |
| Strong pain means the surgery went wrong. | Post‑operative pain is expected; adequate pain control is a sign of proper care. |
| If I feel nauseous, I should stop taking medication. | Nausea is a common side‑effect of opioids and anesthetic gases; anti‑emetics can safely manage it. |
| I can drive as soon as I leave the hospital. | Driving is unsafe until you’re fully alert, usually 24 hours after general anesthesia. |
How to Set Realistic Expectations - Communicating With Your Care Team
Before surgery, ask your anesthetist and surgeon these questions:
- Which type of anesthesia will I receive (general, spinal, regional) and why?
- What are the most common side‑effects for my age and procedure?
- When can I expect to eat, drink, and be discharged?
- What pain‑control plan will be used, and how will nausea be prevented?
- What red‑flag symptoms should prompt a call to the clinic?
Write down the answers, and repeat them with a family member. Having a clear, written plan turns vague anxiety into concrete actions.
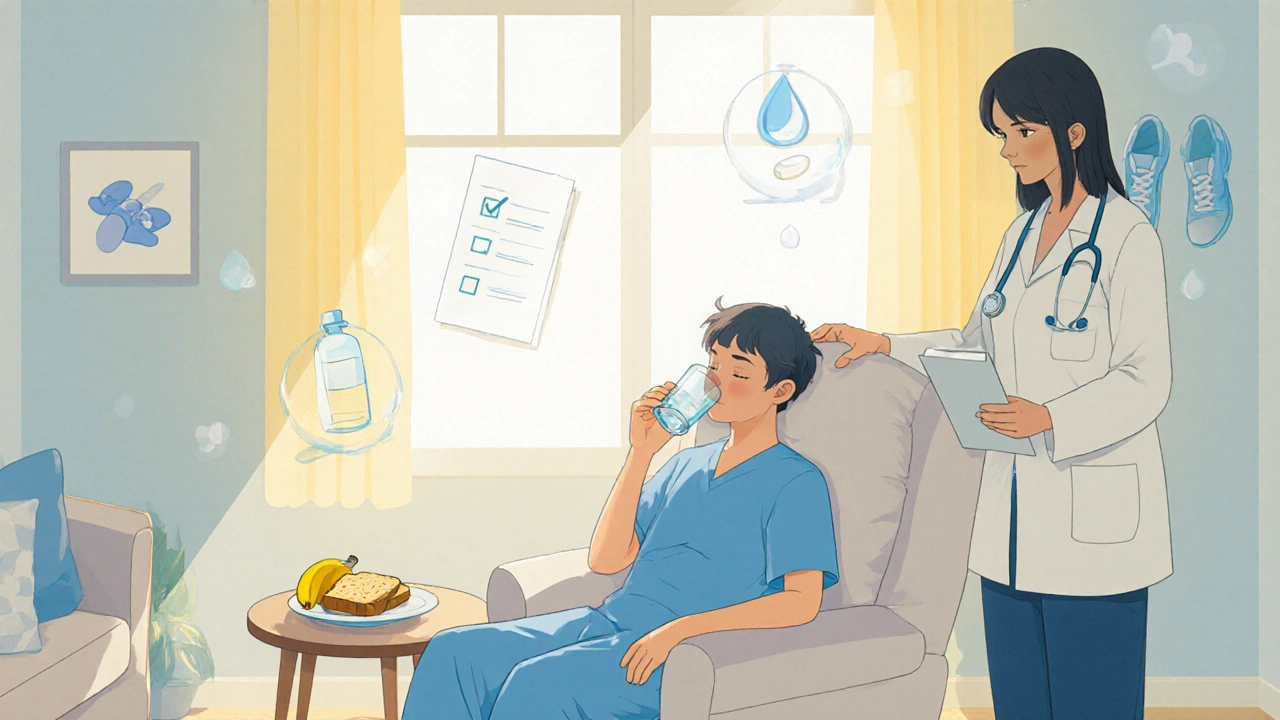
Practical Strategies to Manage Your Recovery
- Hydration: Sip clear fluids every 30 minutes once cleared. Dehydration worsens dizziness and prolongs grogginess.
- Nutrition: Start with bland foods (toast, bananas) before moving to a regular diet. Gentle meals reduce nausea.
- Pain control: Take prescribed analgesics on schedule, not just when pain peaks. Combining non‑opioid meds (acetaminophen, ibuprofen) with opioids can lower the opioid dose needed.
- Mobility: Light walking within the first few hours improves circulation and speeds the clearance of anesthetic agents.
- Sleep hygiene: Dark, quiet rooms and short naps help your brain reset faster.
- Follow‑up calls: Many hospitals schedule a check‑in call 24‑48 hours post‑discharge. Use it to confirm you’re on track.

Red‑Flag Symptoms - When to Call the Surgeon or Anesthetist
Most side‑effects resolve on their own, but these warrant immediate medical attention:
- Severe, worsening abdominal pain or swelling
- Persistent vomiting that prevents fluid intake for more than 12 hours
- High fever (>38.5 °C) or chills
- Sudden shortness of breath or chest pain
- Uncontrolled bleeding or a large amount of drainage from the surgical site
- Confusion, agitation, or inability to recognize familiar people after 48 hours
Quick Checklist Before You Leave the Hospital
- Confirm your discharge medication list and dosing schedule.
- Know the name and dosage of any anti‑emetic prescribed.
- Write down emergency contact numbers (clinic, on‑call anesthetist).
- Arrange a responsible adult to stay with you for at least 24 hours.
- Set up a comfortable recovery space with water, soft lighting, and easy‑reach phone.
Mini FAQ - Answers to the Most Common Questions
How long will the grogginess from anesthesia last?
Most patients feel a “cloudy” head for 1‑2 hours. Full mental clarity usually returns within 24‑48 hours, though older adults may take a bit longer.
Can I drink alcohol during recovery?
Avoid alcohol for at least 48 hours. It interacts with pain meds, worsens dehydration, and can intensify nausea.
When is it safe to drive after a surgery with general anesthesia?
Most guidelines recommend waiting 24 hours and confirming you’re fully alert, have normal vision, and are not taking sedating meds.
What should I do if I feel nauseous but can’t keep medication down?
Sip small sips of clear fluids (water, ginger ale) every 5-10 minutes. If vomiting persists for more than 12 hours, call your care team for an anti‑emetic prescription.
Is it normal to have a sore throat after being intubated?
Yes, the tube can irritate the airway. Warm salt‑water gargles, throat lozenges, and staying hydrated usually help. If the sore throat lasts more than a week or is accompanied by fever, seek medical advice.
Setting realistic expectations isn’t about lowering hopes; it’s about giving yourself a clear roadmap so you can focus on healing instead of worrying about the unknown. By knowing the typical timeline, communicating openly with your care team, and following practical self‑care steps, you’ll turn the waking‑up process into a smoother, safer part of your overall recovery.




Just another boring recovery guide.