Ever felt unusually weak after a long haul of work or a night of heavy drinking and wondered why? The culprit is often hidden in your blood chemistry: low phosphate. This article unpacks the link between hypophosphatemia and muscle weakness, showing you what drives the problem, how doctors spot it, and what you can do to bounce back.
What Is Hypophosphatemia?
Hypophosphatemia is a medical condition characterized by a serum phosphate concentration below the normal reference range (typically < 2.5 mg/dL (0.81 mmol/L) in adults). Phosphate (inorganic phosphate, PO4³⁻) is essential for bone mineralization, cellular signaling, and the production of adenosine triphosphate (ATP), the energy currency of every cell.
How Low Phosphate Undermines Muscle Function
Muscle cells rely on ATP to contract and relax. When phosphate levels drop, ATP synthesis slows, leaving muscle fibers starved for energy. This manifests as generalized fatigue, difficulty climbing stairs, or even severe weakness that mimics neuromuscular disease. In extreme cases, prolonged hypophosphatemia can precipitate rhabdomyolysis, a breakdown of muscle tissue that releases myoglobin into the bloodstream and threatens kidney health.
Beyond ATP, phosphate is a cofactor for enzymes that regulate calcium handling in muscle cells. Disrupted calcium‑phosphate balance can cause abnormal muscle excitability, leading to cramps or paresthesias (tingling sensations).
Common Causes of Low Phosphate
Understanding why phosphate falls helps target treatment. The table below groups the most frequent mechanisms, the typical serum phosphate seen, and the clinical settings where they appear.
| Cause | Mechanism | Typical Serum Phosphate (mg/dL) | Common Clinical Setting |
|---|---|---|---|
| Elevated Parathyroid Hormone (PTH) | Increases renal phosphate excretion | 1.0 - 1.5 | Primary hyperparathyroidism, chronic kidney disease |
| Vitamin D Deficiency | Reduces intestinal phosphate absorption | 1.2 - 2.0 | Limited sun exposure, malabsorption syndromes |
| FGF23‑Mediated Renal Loss | Fibroblast growth factor 23 (FGF23) enhances phosphate wasting | 0.8 - 1.4 | Tumor‑induced osteomalacia, genetic hypophosphatemic rickets |
| Refeeding Syndrome | Insulin surge drives phosphate into cells | <1.0 | Malnourished patients receiving aggressive nutrition |
| Alcoholism | Poor intake + renal losses | 1.0 - 1.8 | Chronic heavy drinkers |
| Diabetic Ketoacidosis (DKA) | Acid‑base shifts cause intracellular phosphate shift | 0.9 - 1.5 | Uncontrolled type 1 diabetes |
Diagnosing Hypophosphatemia
Blood work is the first step. A basic metabolic panel includes serum phosphate, but you may need a repeat test to confirm chronicity. Clinicians also order:
- Serum calcium - to assess concurrent hyper‑ or hypocalcemia.
- Parathyroid hormone (PTH) level - indicates endocrine drive.
- 25‑hydroxyvitamin D - measures vitamin D status.
- FGF23 assay - useful when phosphate loss is suspected from tumor or genetic causes.
- Urine phosphate excretion - differentiates renal loss from poor intake.
Electrolyte trends matter. A sudden drop in phosphate after starting total parenteral nutrition (TPN) often flags refeeding syndrome. In contrast, persistently low values despite adequate intake hint at hormonal or renal drivers.

Managing Muscle Weakness When Phosphate Is Low
Therapy targets two fronts: correcting phosphate and supporting muscle recovery.
- Phosphate Repletion: Oral sodium phosphate tablets (250‑500 mg elemental phosphate) are first‑line for mild‑to‑moderate cases. For severe or symptomatic patients (e.g., <1.0 mg/dL with weakness), IV phosphate (often as potassium phosphate) is administered under cardiac monitoring to avoid hypocalcemia or hyperkalemia.
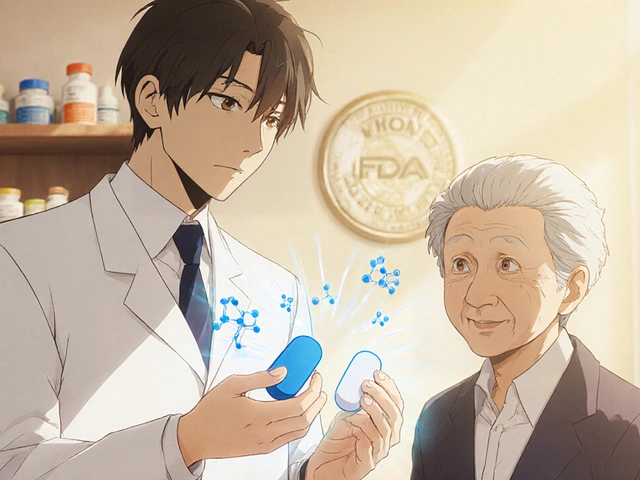
- Address Underlying Cause: If PTH is high, treat hyperparathyroidism surgically or with calcimimetics. Vitamin D deficiency requires cholecalciferol or calcitriol supplementation (typically 800-2000 IU daily). For FGF23 excess, phosphate‑binding agents and, in some cases, monoclonal antibodies (burosumab) are effective.
- Nutrition Support: Encourage foods rich in phosphate - dairy, meats, nuts, legumes - while balancing renal restrictions if chronic kidney disease is present.
- Physical Rehabilitation: Light resistance exercises and physiotherapy improve muscle strength once phosphate levels stabilize. Start with low‑impact activities (e.g., walking, stationary cycling) and progress as tolerated.
Monitoring is crucial. Repeat serum phosphate every 12-24 hours during IV repletion and weekly thereafter for oral therapy. Watch for rebound hypophosphatemia, especially in patients with high urinary losses.
Prevention and At‑Risk Populations
Certain groups need extra vigilance:
- Critically ill patients on TPN or dialysis - early phosphate checks prevent refeeding injury.
- Chronic alcohol users - supplement with multivitamins containing phosphate and vitamin D.
- Pregnant women - fetal bone development relies on maternal phosphate; prenatal labs include phosphate screening.
- Children with genetic rickets - lifelong monitoring and burosumab therapy are recommended.
Proactive measures include regular electrolyte panels, adequate dietary intake, and avoiding abrupt nutritional shifts in malnourished patients.
Related Concepts and Next Steps
Understanding hypophosphatemia opens doors to a broader health picture. Explore topics such as:
- Bone Mineral Density - how low phosphate weakens bones over time.
- Electrolyte Disorders - the interplay between phosphate, potassium, and magnesium.
- Renal Tubular Acidosis - a condition that frequently co‑exists with phosphate wasting.
These topics give you a roadmap to comprehensively manage metabolic health.
Frequently Asked Questions
What serum phosphate level defines hypophosphatemia?
In adults, a serum phosphate below 2.5 mg/dL (0.81 mmol/L) is generally considered hypophosphatemic. Levels under 1.0 mg/dL often produce noticeable muscle weakness.
Can diet alone fix low phosphate?
Mild cases may improve with phosphate‑rich foods like dairy, meat, nuts, and legumes. Severe or symptomatic hypophosphatemia usually requires oral or IV supplementation because dietary intake alone cannot rapidly raise serum levels.
Why does refeeding syndrome cause a phosphate drop?
When a starving patient receives carbohydrates, insulin spikes and drives phosphate into cells for ATP generation. The sudden intracellular shift leaves the bloodstream depleted, often below 1.0 mg/dL.
Is muscle weakness from low phosphate reversible?
Yes. Once phosphate levels are restored and the underlying cause addressed, most patients regain strength within days to weeks. Persistent weakness may indicate additional neuromuscular issues that need separate evaluation.
Should I have my phosphate checked regularly?
If you have risk factors-chronic kidney disease, heavy alcohol use, malnutrition, or endocrine disorders-annual or bi‑annual serum phosphate testing is wise. Otherwise, routine panels during yearly physicals usually include it.
Can low phosphate affect the heart?
Severe hypophosphatemia can impair myocardial contractility and cause arrhythmias, especially when combined with low potassium or calcium. Prompt correction is essential in critical care settings.



Well i guess my muscles finally got the memo.