For millions of people with obstructive sleep apnea, the CPAP machine is a nightmare - not because it doesn’t work, but because it’s impossible to live with. The mask digs into your face, the hose tangles in your sheets, and the constant air pressure feels like choking. If you’ve tried CPAP and walked away, you’re not alone. About 3 in 10 people give up on it within the first year. But what if there was another way? Something that doesn’t require a mask, doesn’t need daily cleaning, and works while you sleep - without you even thinking about it?
What Is Upper Airway Stimulation?
Upper airway stimulation (UAS) is a surgically implanted device that treats sleep apnea by gently waking up your tongue’s muscles when you breathe in. It’s not a cure, but it’s a game-changer for people who can’t tolerate CPAP. The most common system, called Inspire, was approved by the FDA in 2014 and has since helped over 200,000 people worldwide. Unlike CPAP, which pushes air into your throat, UAS works from the inside. It senses when you’re inhaling and sends a tiny electrical pulse to the nerve that controls your tongue. That pulse moves your tongue forward, keeping your airway open so you can breathe without snoring or gasping.
The device has three parts: a small generator implanted under your chest, a sensing wire that monitors your breathing, and a stimulation wire that wraps around the nerve behind your jaw. All of it’s hidden under your skin. You don’t feel it during the day. At night, you turn it on with a small remote - like flipping a light switch. It turns off automatically when you wake up.
Who Is a Good Candidate?
This isn’t for everyone. You need to meet specific criteria to qualify. First, you must have moderate to severe sleep apnea - an AHI (apnea-hypopnea index) between 15 and 100 events per hour. Second, you’ve already tried CPAP and couldn’t stick with it. Third, your body mass index (BMI) must be under 35. (In 2023, the FDA expanded eligibility to include people with BMI up to 40, which opened the door for more patients.)
There are also anatomical requirements. Your airway must not be completely blocked when you’re asleep, and your soft palate can’t collapse inward in a circular pattern. Doctors check this with a special sleep endoscopy - a quick, sedated exam that shows exactly where your airway closes. If your tongue is the main problem, UAS works great. If your throat collapses from the sides, it won’t help.
You also need to be at least 22 years old. It’s not approved for teens or younger adults. And if more than 25% of your breathing pauses are central apneas (caused by your brain not signaling your body to breathe), UAS won’t work. It only treats obstructive sleep apnea - the kind caused by physical blockage.
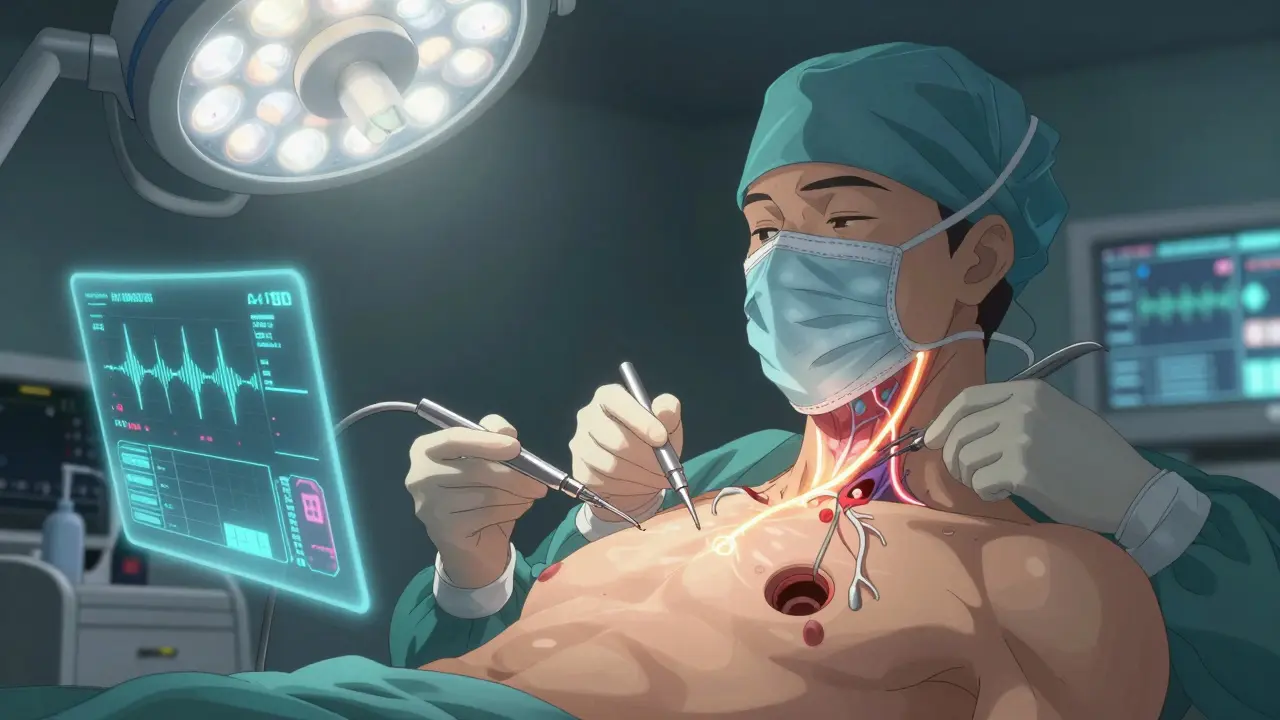
How Does the Surgery Work?
The procedure is done as an outpatient surgery under general anesthesia. You go home the same day. Three small incisions are made: one near your collarbone to place the generator, one under your jaw to place the stimulation wire on the hypoglossal nerve, and one in your neck to place the breathing sensor. The whole thing takes about two to three hours.
Recovery is quicker than you’d expect. Most people are back to light activities within five to seven days. You might feel some soreness or swelling, but it’s nothing like traditional throat surgeries. There’s no cutting into your palate or removing tissue. The device is fully reversible - if you ever decide to remove it, the hardware can be taken out without lasting damage to your nerves or muscles.
Activation doesn’t happen right away. You wait about four weeks for healing. Then, your sleep doctor programs the device using a handheld remote and a computer. They’ll adjust the strength of the stimulation over several visits until it’s just right - not too weak, not too strong. It’s like tuning a radio. You’ll have follow-ups at 1, 3, 6, and 12 months to make sure it’s still working well.
How Effective Is It?
The data speaks for itself. In the STAR trial - the largest long-term study on UAS - patients saw their AHI drop from an average of 29.3 events per hour to just 9.0 after one year. That’s a 68% reduction. Two-thirds of patients had their AHI cut in half or more. Even better, 86% of users say they prefer UAS over CPAP. On patient forums, common comments include: “My wife says I stopped snoring completely,” and “I feel like I’m sleeping for the first time in 15 years.”
Bed partners notice the difference too. At the four-year mark, 85% of partners reported either no snoring or only soft snoring. Daytime sleepiness improved significantly. People reported better focus, less irritability, and more energy. These aren’t minor perks - they’re life-changing.
Complications are rare. The major complication rate is under 0.5%. Most side effects are mild: temporary tongue weakness (seen in 5% of patients during the first few months), minor swelling, or irritation at the incision sites. A small number of people report forgetting to turn the device on - which is the biggest behavioral hurdle. But once it becomes part of your nightly routine - like brushing your teeth - it’s effortless.
How Does It Compare to CPAP and Other Surgeries?
CPAP is still the gold standard - if you can use it. But for those who can’t, UAS wins on adherence. People use UAS an average of 7.5 hours a night. CPAP users average just 4.2 hours, and many stop entirely. UAS doesn’t require masks, hoses, or daily cleaning. It’s silent, invisible, and doesn’t dry out your mouth.
Compared to older surgeries like uvulopalatopharyngoplasty (UPPP), UAS is far more effective. UPPP removes tissue from the throat - and even then, it only works for about half of patients. It’s painful, has a long recovery, and often doesn’t fix the problem. UAS works without cutting anything. It’s adjustable, reversible, and targets the exact cause of obstruction: the tongue falling back.
Oral appliances - mouthpieces that push your jaw forward - are another option. They’re less invasive than surgery, but they don’t work for everyone, especially those with severe apnea. UAS has a higher success rate in moderate to severe cases and doesn’t affect your bite or teeth over time.

Cost and Insurance Coverage
The total cost of the procedure - device, surgery, hospital fees - ranges from $35,000 to $40,000. That sounds steep, but it’s comparable to the long-term cost of CPAP. Think about it: CPAP machines need replacing every 5 years. Masks, filters, and tubing cost hundreds a year. Follow-up visits, sleep studies, and replacement parts add up. Over a decade, many patients spend more than $30,000 on CPAP-related expenses.
Insurance coverage has improved dramatically. As of 2023, 95% of Medicare patients and 85% of privately insured patients have coverage for UAS therapy. Most insurers require proof of CPAP failure before approving the implant. Your sleep specialist will help you navigate the paperwork. The Inspire Patient Support Program also offers financial counseling and payment plans.
What’s Next for This Technology?
The field is moving fast. Researchers are using AI to analyze airway scans and predict who will respond best to UAS - before surgery. Newer versions of the device are smaller, with longer battery life. Some prototypes can even adjust stimulation automatically based on sleep position or alcohol intake.
Doctors are also exploring whether UAS can help people with mild sleep apnea who struggle with CPAP. Early trials are promising. And as more surgeons become trained in the procedure, access is expanding beyond major medical centers. In Australia, the therapy is available in select hospitals in Melbourne, Sydney, and Brisbane, with more clinics expected to adopt it in 2026.
Final Thoughts
If you’ve given up on CPAP and are still waking up exhausted, UAS might be your best shot at real, lasting relief. It’s not a magic bullet - you still need to be a good candidate, and you still need to remember to turn it on. But for the right person, it’s the difference between living with sleep apnea and finally sleeping like a normal person.
It’s not about giving up on treatment. It’s about finding the right one. And for thousands of people, that’s now possible without a mask, without a hose, and without giving up on sleep.
Is upper airway stimulation the same as a CPAP machine?
No. CPAP uses pressurized air delivered through a mask to keep your airway open. Upper airway stimulation (UAS) is a surgically implanted device that gently stimulates the nerve controlling your tongue, moving it forward to prevent blockage. UAS doesn’t require a mask, hose, or external machine. It works silently from inside your body.
Can I still use a CPAP after getting UAS?
Yes, but most people don’t need to. Once UAS is properly programmed and working, it effectively replaces CPAP. Some patients keep their CPAP machine as a backup for travel or if the device is turned off temporarily. But in daily use, UAS is designed to be the sole therapy.
Does the implant set off metal detectors or affect MRIs?
The generator may trigger airport security alarms, but you’ll be given a medical ID card to show security personnel. As for MRIs, most modern Inspire devices are MRI-compatible under specific conditions - usually for head and neck scans at 1.5 Tesla or lower. You must inform your radiologist about the implant before any scan. Full-body MRIs at higher strengths are still not recommended.
How long does the battery last?
The generator’s battery lasts about 11 years on average. When it starts to run low, your doctor will schedule a simple outpatient procedure to replace the generator - similar to replacing a pacemaker. The stimulation and sensing wires stay in place. No major surgery is needed.
What if I gain weight after the implant?
Weight gain can reduce the effectiveness of UAS. While the device still works, higher body fat can increase airway collapse. If your BMI rises above 40, your doctor may recommend combining UAS with lifestyle changes or even revisiting CPAP. Maintaining a healthy weight helps ensure long-term success.
Is this covered by Medicare in Australia?
As of 2025, Medicare in Australia does not yet fully cover upper airway stimulation for sleep apnea. However, some private health insurers offer partial coverage under certain extras or hospital policies. Patients often pay out-of-pocket or use payment plans offered by the manufacturer. Coverage is expected to expand as more clinical data becomes available locally.





