For those managing edema or hypertension, Lasix has been a well-known diuretic option. However, it's not the only choice available in 2024. Here, we explore six alternatives that can serve individuals with varied medical needs and preferences. Whether you're seeking enhanced effectiveness or specific benefits like potassium retention, these options provide viable pathways. Selecting the right diuretic involves weighing the benefits against potential side effects, and being informed is the first step towards making the best decision for your health.
Torsemide
Torsemide stands out as an important alternative to the well-known Lasix, especially for those grappling with conditions like congestive heart failure. Unlike some of its counterparts, Torsemide's unique mechanism blocks sodium and chloride reabsorption more efficiently in the kidneys. This leads to a rapid increase in the excretion of water, sodium, and chloride. Available in both oral tablet and injectable forms, it's known for having high bioavailability, around 80%. It becomes a compelling option for patients due to its potency—twice as effective as furosemide when measured on a milligram-per-milligram basis. Users often opt for Torsemide due to its potential benefit in reducing hospitalization rates and enhancing clinical outcomes.
For individuals with congestive heart failure, better outcomes translate to improved quality of life. Medical communities have noted how Torsemide may offer more predictable diuresis and absorption compared to Lasix. Yet, like any medication, it demands careful handling. Healthcare providers often highlight the need for regular monitoring of electrolytes and kidney function, since improper management might lead to unwanted effects like excessive urination or dizziness. For anyone considering this medication, discussion with a healthcare provider is necessary to align treatment goals with Torsemide's capabilities.
“In studies, Torsemide has demonstrated a stronger impact on fluid balance in heart failure patients, reducing rehospitalizations,” says Dr. Steven Nissen, a renowned cardiologist.
Torsemide might not be the first choice for everyone dealing with high blood pressure or edema. However, those who need effective long-term management can benefit significantly from its superior absorption profile. It's essential for patients switching from other diuretics to be aware of these possible side effects and the necessity of regular health checks. Evaluations often include monitoring blood pressure and kidney function. This helps ensure that the fluid loss doesn't extend to critical electrolytes necessary for the body's equilibrium. Since it acts as a powerful loop diuretic, medical practitioners discourage its usage without professional oversight.
The healthcare community's experience with Torsemide suggests it might serve certain patient subsets better than Lasix. Its stronger potency and ability to help in heart failure without repeated hospital visits marks it as a drug worth considering. That being said, effective use requires vigilance in observing how it influences body chemistry over time. Exploring its interactions with other medications, and ensuring a balance between treatment goals and patient conditions, ultimately shapes its role in modern treatment strategies.
Bumetanide: A Potent Diuretic Alternative
Bumetanide stands out as a potent alternative to Lasix, known for its effectiveness in treating edema that often accompanies conditions like congestive heart failure, chronic renal failure, and nephrotic syndrome. This loop diuretic mirrors Lasix’s mechanism by increasing urine production to alleviate excess fluid from the body's tissues. Available as oral tablets and injectable solutions, Bumetanide provides a flexible treatment option for various healthcare settings. Its practical applications extend beyond simple water retention issues, providing relief to those who may not respond adequately to other treatments. As a consequence, it's an attractive alternative in difficult-to-treat cases, offering a powerhouse of potential where other diuretics may fall short.
Despite its efficacy, Bumetanide requires careful usage due to the possible risk of dehydration, electrolyte imbalances, and kidney complications if unmonitored. This makes regular check-ups an essential part of using this medication. Hydration levels, electrolyte status, and kidney functions need to be carefully assessed throughout the treatment to ensure the benefits outweigh the risks. Its high potency makes it a preferred choice when more aggressive fluid management is necessary, but this comes hand-in-hand with the responsibility of vigilant medical oversight. By tailoring Bumetanide use to individual patient needs, healthcare providers can optimize outcomes and minimize potential adverse effects.
Several studies highlight Bumetanide’s efficacy, particularly in patients who are unresponsive to Furosemide, another loop diuretic. This feature underscores its role as a second-line treatment in resistant cases of edema. In clinical practice, utilizing Bumetanide can contribute to significant improvements in patient comfort and symptom management, offering a strategic advantage in complex therapeutic scenarios. It boasts a higher degree of potency on a milligram-to-milligram comparison, allowing for dose adjustments tailored to the patient's specific response and tolerance levels. However, this does not diminish the necessity for precise dose calculations and frequent assessments by healthcare providers to maintain a safe therapeutic window.
As a reflection of public and professional regard, a quote from renowned nephrologist Dr. Emily Winters encapsulates the significance of Bumetanide, "In patients with heart failure where fluid overload is challenging to control, Bumetanide often provides the solution that restores function and life quality." Her insight underscores the medication’s value as a formidable ally in the ongoing battle against debilitating fluid retention. Such endorsements from experienced practitioners help validate Bumetanide’s place within modern medical protocols, affirming its capability to address specific medical challenges encountered in diuretic therapies.

Chlorthalidone
When we talk about effective alternatives to Lasix, Chlorthalidone often finds a mention, especially noted for its role in treating hypertension and edema. Known in medical circles as a thiazide diuretic, Chlorthalidone stands apart because it curbs the kidney’s ability to retain sodium and water, which increases urine output. This mechanism plays a vital role in shedding excess fluid from the body, which typically benefits those with high blood pressure or swelling-related conditions.
A fascinating fact about Chlorthalidone is its recommendation by the American Heart Association as a first-line medication for hypertension. This speaks volumes about its efficacy and dependability, particularly for people beginning treatment for high blood pressure. The way it manages blood pressure is quite methodical, blending its action over time to ensure not only the immediate reduction of pressure but extending its benefits over a longer period.
Many find Chlorthalidone to be a superhero in battling heart issues because it can reduce the risk of cardiovascular events. A study found that patients on this medication saw a notable drop in heart attack and stroke occurrences, showing its preventive prowess. What’s interesting is the dual role it plays, offering benefits both for active problems like edema and as a preventive measure for more severe heart-related conditions.
Dr. Emily Hanson, a cardiovascular specialist, notes, "Chlorthalidone's efficacy in preventing hypertension-related complications is a game-changer in cardiac care."
Of course, while its benefits are enticing, like any medication, Chlorthalidone isn't free from potential pitfalls. Some might face challenges like electrolyte imbalance, notably low potassium levels. This often necessitates regular monitoring, ensuring levels stay safe and balanced. The follow-up care might deter some, but it’s an essential blueprint for maintaining health while on Chlorthalidone. This need for vigilance underscores the importance of personalized care in medication management.
For many patients, especially those starting their hypertension journey, Chlorthalidone is more than a medication—it's a reliable partner. With consistent use, most experience noticeable improvements in their condition, making it a cornerstone in hypertension treatment plans.
Spironolactone
When it comes to the realm of diuretics, Spironolactone stands out for its unique mode of action. Unlike other diuretics, Spironolactone is a potassium-sparing medication. This characteristic makes it particularly advantageous for individuals who need to retain potassium in their body while eliminating excess fluid. The body’s balance of potassium is crucial for maintaining heart and muscle function, and the fact that Spironolactone helps preserve this balance sets it apart from other options like Lasix. Typically used in edema and hypertension, it blocks the effects of the hormone aldosterone, leading to sodium and water being expelled from the body efficiently. Interestingly, Aldactone, the brand name for Spironolactone, was first discovered over 60 years ago and has since been a trusted choice recommended by healthcare professionals worldwide. Its ability to mitigate fluid build-up also helps reduce the workload on the heart, proving beneficial particularly in heart failure patients.
Moreover, Spironolactone is commonly employed in treating resistant hypertension—a condition where blood pressure remains high despite the use of multiple medications. By combining it with other diuretics, it tackles the issue on multiple fronts, offering a collaborative approach in medication regimens. A report by the Mayo Clinic noted, “The role of Spironolactone in resistant hypertension is significant and well-documented, offering a 'last-line' defense for patients experiencing water retention and related issues.” Such endorsements from significant health institutions underline its importance in contemporary medicine. Many patients report experiencing not only a reduction in blood pressure but also the side benefit of acne treatment, as Spironolactone works as an anti-androgen by reducing the level of male hormones, which in turn decreases sebum production and acne.
However, it's important to remain aware of possible side effects. One primary concern with Spironolactone is hyperkalemia—the condition where there is too much potassium in the blood. This can lead to complications if not monitored regularly. Hence, individuals taking this medication must undergo regular blood tests to ensure potassium levels remain within safe limits. Patients may also experience breast tenderness, hormonal changes, or stomach discomfort. Despite these potential side effects, the benefits of Spironolactone often outweigh the risks, providing vital relief from conditions like heart failure and high blood pressure. An interesting factworthy of note is that the drug has even been used off-label to treat female pattern hair loss due to its hormonal modulation properties. Currently, healthcare providers recommend careful dosage adjustments based on the individual patient’s needs and responses, ensuring the maximum therapeutic benefit while minimizing adverse effects.

Hydrochlorothiazide
Hydrochlorothiazide stands out as a staple in the world of diuretics, often finding its way into prescription pads for those dealing with hypertension and edema. It's been around for years, proving to be effective in tackling these common issues by gently coaxing the kidneys to release sodium and water, lowering blood volume, and ultimately easing blood pressure. This simplicity in its mechanism makes it a first-line treatment in many cases. Most notably, when doctors prescribe Hydrochlorothiazide, they do it with confidence, aligning with guidelines put forth by respected bodies like the American Heart Association.
Part of what makes Hydrochlorothiazide so prevalent is its dual capability to manage high blood pressure and fluid retention, tagged as edema. These two conditions, often walking hand in hand, find a manageable conductor in Hydrochlorothiazide. While effective, its use is not without the need for vigilance. Patients must regularly monitor their blood electrolyte levels, as the medication can alter these balances, tipping the scale particularly with potassium. An imbalanced electrolyte profile can lead to unwanted effects, from muscle cramps to fatigue or more serious heart irregularities.
In recent years, newer studies have often put Hydrochlorothiazide's effectiveness in the spotlight compared to its peers. Instances of improved long-term heart health outcomes in hypertensive patients are worth noting. According to a study published in the Journal of the American Medical Association, "Hydrochlorothiazide continues to show promising results in mitigating risks associated with cardiovascular complications in hypertension patients." With such a vast consumer population, those prescribed Hydrochlorothiazide need to maintain a dialogue with their healthcare providers, ensuring that the treatment remains effective while sidestepping potential pitfalls such as low potassium.
"In managing hypertension, Hydrochlorothiazide remains a reliably effective choice," Dr. Emily Carter, a cardiologist, noted during a health symposium last year, highlighting its continued relevance.
Also intriguing is the role Hydrochlorothiazide plays when combined with other medications. Often seen accompanying medications like beta-blockers or ACE inhibitors, it complements these by enhancing their efficacy to control pressure and prevent complications better. This combination therapy has been shown to help people maintain stable blood pressure levels more robustly than single-drug use, making it an important strategy in comprehensive hypertension management.
For those considering Hydrochlorothiazide, or already on it, integrating lifestyle changes can amplify the benefits. Simple actions like maintaining a diet rich in fruits and vegetables and engaging in regular, moderate exercise can enhance its effectiveness. The key is striking a balance where medication and lifestyle join forces, offering a one-two punch against high blood pressure and excess body fluid. While Hydrochlorothiazide is a trusted ally against hypertension and edema, like any tool, its power is best harnessed in collaboration with broader health strategies, echoing the sentiment that medicines often work best in tandem with other healthy habits.
Metolazone
Metolazone is a renowned diuretic particularly valued for its role in treating edema associated with conditions like congestive heart failure and nephrotic syndrome. Known for its efficiency in encouraging substantial urine output, Metolazone helps the body rid itself of excess water and salt. By doing so, it alleviates the burden on the heart and eases the swelling in tissues, which can be debilitating if not managed effectively. Many patients and healthcare providers choose Metolazone when furosemide-based treatments, such as Lasix, prove insufficient.
One of the remarkable qualities of Metolazone is its versatility in conjunction with other diuretics—a common practice when heart failure or severe kidney disorders are involved. Such strategic combinations enhance the fluid-removal process, tackling more pronounced symptoms through diversified pathways. However, with this powerful action comes the need to monitor it closely. Regular assessment of the patient's electrolyte levels is imperative, as Metolazone, like many diuretics, may lead to an imbalance, notably affecting potassium levels. These checks ensure that while addressing fluid retention, the body does not veer into an undesirable state of dehydration or electrolyte imbalance.
In practice, the use of Metolazone often involves rigorous observations and patient-specific adjustments, which can seem daunting yet necessary. Doctors typically initiate treatment with a tangible balance, adjusting doses based on individual response and underlying health conditions. This precision ensures the treatment remains effective without tipping into excessive fluid loss. According to the Nephrology and Clinical Journal, "Metolazone's unique properties complement the therapeutic needs in heart failure management when prescribed diligently."
Moreover, the scenario where Metolazone becomes essential typically reflects a stage where conventional treatments require a boost. In such cases, it can significantly contribute to reducing hospitalization rates associated with heart failure. In some instances, healthcare teams may leverage Metolazone's action to prepare patients for surgery by optimizing fluid balance pre-operatively. This ability to adapt its role underscores why Metolazone retains prominence among diuretics, making it indispensable in particular therapeutic niches.
In summary, while Metolazone serves crucial purposes for specific ailments, it demands a high degree of care and attention—from patients and practitioners alike. The balance of benefit and risk is ever-present, but with meticulous management, it becomes a beacon of effective diuretic action, helping those who need it reclaim a more stable, healthier life. Its standing in modern medicine is a testament to its unmatched utility in highly specialized situations where alternative treatments might falter.

Conclusion
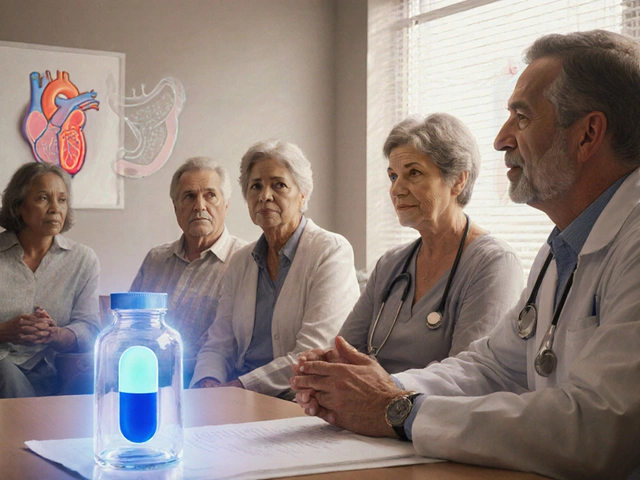
As we bring this exploration of Lasix alternatives to a close, it's evident that each of the options examined offers unique benefits for managing edema and hypertension. Health care is deeply personal, and what works for one individual might not be ideal for another. This is why it is so vital to have a range of choices, each tailored to meet different health needs. In particular, Torsemide excites with its potential in treating congestive heart failure with notable effectiveness and lower hospitalization rates, which might serve those who need stable, reliable interventions.
Bumetanide stands out for those unable to achieve their goals with furosemide, offering a trustworthy substitute. In contrast, Chlorthalidone and Hydrochlorothiazide emerge as front-line soldiers in the battle against hypertension, owing to their tried-and-true action mechanisms. On another note, for patients concerned with maintaining adequate potassium levels, Spironolactone is a superb option that safeguards against potential deficiency while still being effective in diuresis. Each medication has its set of pros and cons, including the need for vigilant monitoring of electrolytes and kidney function, which is an unavoidable part of using diuretics.
A poignant testimonial from the American Journal of Cardiology highlights,
"The ultimate goal in diuretic selection is not only symptom alleviation but improved quality of life, and diverse options like these enrich our capacity to achieve that."This underscores the significance of making an informed decision with the guidance of a healthcare provider. As our options evolve, it is crucial to remember the importance of regular follow-ups and blood tests to ensure these medications perform optimally without introducing undue risk.
| Alternative | Strength | Key Consideration |
|---|---|---|
| Torsemide | Effective for CHF | Monitor kidney function |
| Bumetanide | Great for refractory cases | Risk of dehydration |
| Chlorthalidone | First-line for hypertension | Electrolyte management |
| Spironolactone | Potassium-sparing | Hyperkalemia risk |
| Hydrochlorothiazide | Good for long-term use | Low potassium levels |
| Metolazone | Refractory edema | Fluid status monitoring |
The choice of a diuretic is indeed multifaceted, but with the right guidance and understanding, it can significantly impact one’s quality of life. The advances and options available in 2024 reflect our growing understanding of cardiovascular health, and each step forward holds promise for improved patient outcomes. As always, consult your physician to decide the best course of action.



It’s no accident that the big pharma lobby has a vested interest in keeping Lasix as the headline diuretic,; the way they patent every slight variant,; the way they fund key opinion leaders,; and the way they lobby regulatory agencies to stifle generic competition – all point to a coordinated effort to control the market,; not to mention the hidden clauses in physician‑payment agreements that subtly steer prescribing habits toward the most profitable brands,; which, of course, leaves patients with fewer affordable choices and a false sense of safety about the “standard” therapy.