Side Effect Tolerance Calculator
Predict Your Side Effect Tolerance
Based on medical research about differential tolerance, predict which side effects might fade over time.
Select your medication and side effect to see when tolerance might occur.
How This Works
This calculator uses real-world data from the article:
- Opioids: 90% of patients still have constipation after weeks while nausea fades
- SSRIs: 73% stop nausea in 3 weeks but 58% still have sexual side effects
- Benzodiazepines: sedation fades in 7-14 days while anxiety relief persists
Tolerance depends on differential tolerance—different body systems adapt at different rates.
Have you ever started a new medication and felt awful the first few days-nausea, dizziness, exhaustion-only to find those symptoms vanished after a week or two? Meanwhile, another side effect, like constipation or sexual dysfunction, stuck around like an uninvited guest? It’s not just in your head. This isn’t bad luck or bad medicine. It’s tolerance-and it’s happening in your cells.
When you take a drug repeatedly, your body doesn’t just get used to it. It actively rewires itself to counteract the drug’s effects. Some parts of your body adapt quickly. Others don’t. That’s why nausea fades but constipation doesn’t. Why dizziness disappears but fatigue lingers. This isn’t random. It’s biology, and it’s predictable-if you know what to look for.
How Your Body Learns to Ignore Drugs
Tolerance isn’t about your body becoming stronger. It’s about your body becoming smarter at undoing what the drug does. There are three main ways this happens.
First, your liver gets faster. Many drugs are broken down by enzymes called cytochrome P-450. When you take a drug like barbiturates or alcohol every day, your liver says, “Oh, you’re doing this again?” and starts producing more of these enzymes. In some cases, alcohol can boost its own metabolism by up to 300%. That means the drug gets cleared from your system faster, so you feel less of it. This is called pharmacokinetic tolerance.
Second, your brain changes its receptors. Think of receptors like locks, and drugs like keys. Over time, your body might reduce the number of locks (receptor downregulation), make the locks harder to turn (lower binding affinity), or even change the shape of the lock itself. Opioids, for example, can cause a 20-50% drop in receptor numbers in certain brain areas. Benzodiazepines do the same thing with GABA receptors. This is pharmacodynamic tolerance-and it’s why the same dose stops working the same way.
Third, your cells rewire their internal wiring. Chronic alcohol use, for instance, doesn’t just reduce GABA receptors-it changes which subunits make up those receptors. It increases the R2B subunit in NMDA receptors by 40-60%. That’s not a small tweak. That’s a full system upgrade. The brain is trying to balance out the drug’s effects. It’s like turning down the volume on one speaker while leaving the bass cranked up.
Why Some Side Effects Vanish-and Others Don’t
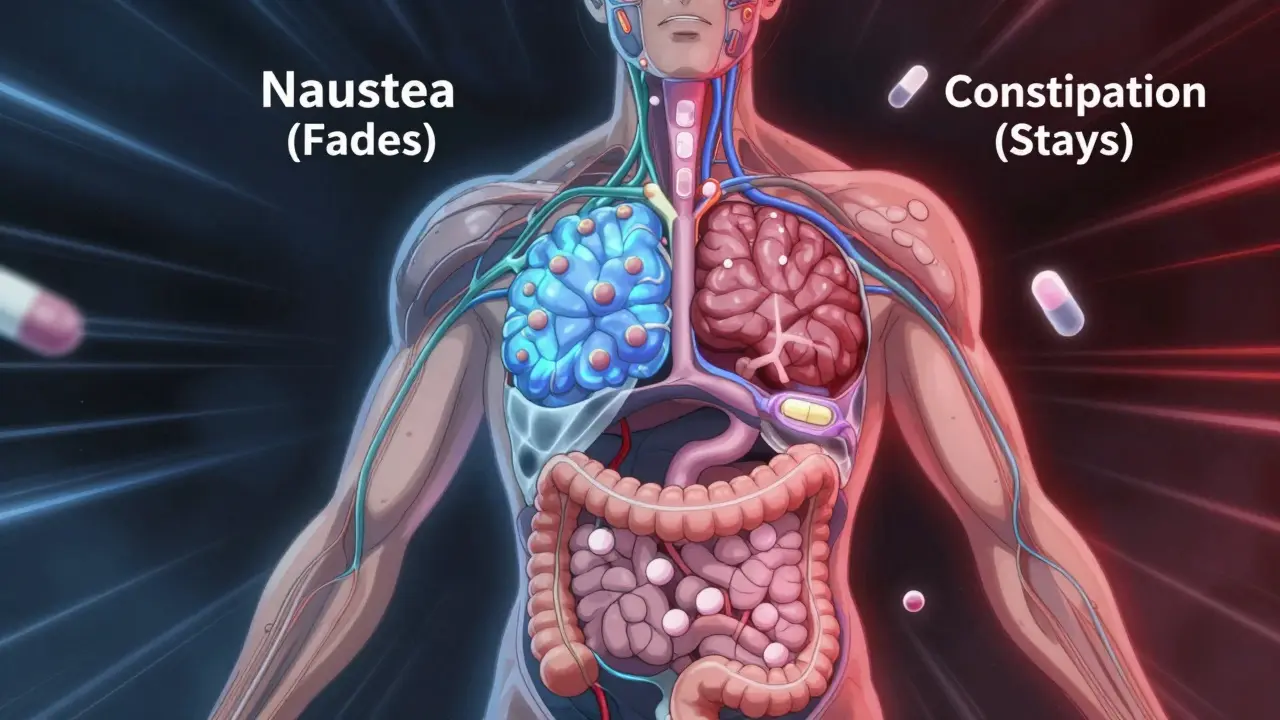
Not all side effects fade at the same speed. This is called differential tolerance. It’s one of the most important-and overlooked-concepts in medicine.
Take opioids. After just 2-3 doses, people start to feel less drowsy. Sedation drops by 70-80% within a week. But constipation? It barely budges. Studies show 90% of patients still have it after weeks of use. Why? Because the receptors that cause drowsiness are in the brainstem. The ones causing constipation are in the gut. Different locations. Different receptors. Different adaptation rates.
Same with benzodiazepines. The sedative effect fades in 7-14 days. But the anxiety relief? Stays strong. That’s why doctors can keep patients on low doses long-term for panic disorder without losing effectiveness. The brain adapts to the calming effect differently than the sleepy effect.
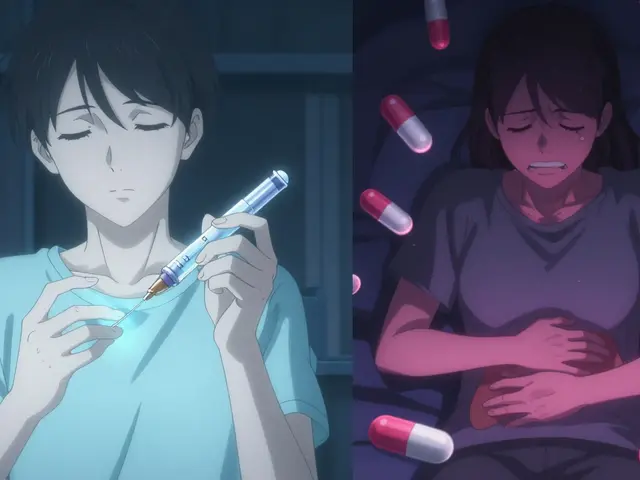
Antidepressants like SSRIs show this too. Within 2-3 weeks, 73% of users stop feeling nauseous. But sexual side effects? They stick around for 58% of people. Why? Because serotonin receptors in the gut adapt quickly. The ones in the brain regions controlling arousal? Not so much.
Even beta-blockers, used for high blood pressure, follow this pattern. Fatigue from the first week? Usually gone in 3 months. Blood pressure control? Stays steady. The heart adjusts. The blood vessels don’t.
What the Data Says: Real Patient Experiences
Real people aren’t just numbers. They’re sharing this pattern online-and it’s consistent.
- On Reddit’s r/ChronicPain, 78% of 1,245 users said opioid-induced nausea disappeared in 5-7 days. But 92% still had constipation.
- Drugs.com reviews of 4,327 people on pregabalin showed 65% had less dizziness after 10-14 days. By day 21, 82% said it was completely gone.
- 2,145 patients on SSRIs reported 73% lost nausea within 3 weeks. But 58% still struggled with sexual side effects months later.
- MS patients on interferon beta-1a: 68% said initial fatigue faded in 4-6 weeks. Injection site pain? Still there.
One user wrote: “Started oxycodone for back surgery-vomiting stopped after day 3. Constipation never went away.” Another: “The dizziness that made me fall the first week is gone. But I still can’t maintain an erection.” These aren’t rare. They’re routine.

Why This Matters for Your Health
Understanding tolerance isn’t just academic. It changes how you take care of yourself.
If you’re on an opioid and still throwing up after a week, don’t assume you’re doing something wrong. Your body is adapting. But if you’re still constipated? That’s not tolerance. That’s a side effect that needs action. Doctors should prescribe laxatives from day one-not wait until you’re in pain.
If you’re on an SSRI and feel worse after two weeks, you might think it’s not working. But if your nausea is gone and your mood is improving? That’s a sign it’s working. The side effects you’re still feeling might not go away-and that’s okay. You can manage them.
And if you’re told to “just push through” the side effects? That’s outdated thinking. Tolerance isn’t a test of endurance. It’s a biological process. Some things fade. Some don’t. Knowing the difference helps you make smarter choices.
When Tolerance Gets Dangerous
Here’s the risk: when side effects fade, people think, “This must be working better.” So they increase the dose. That’s dangerous.
With opioids, reducing nausea doesn’t mean your body is less sensitive to respiratory depression. You can still overdose-even if you feel fine. That’s why some people die after increasing their dose because “they didn’t feel the side effects anymore.”
Same with benzodiazepines. If sedation fades, you might think you can drive. But your reaction time might still be impaired. Your brain adapted to the drowsiness-not the motor control.
And don’t confuse tolerance with dependence. Just because you feel less nausea doesn’t mean you’re addicted. Tolerance is a physiological change. Addiction involves cravings, loss of control, and compulsive use. They’re related, but not the same.
What’s New in Tolerance Research
Science is catching up. In 2023, the FDA approved a new combo drug-naltrexone and bupropion-that specifically targets opioid-induced nausea. Clinical trials showed a 45% drop in persistent nausea compared to regular opioids.
Researchers are also testing polymer-coated pills that release drugs slowly. Early results show 60% less tolerance development to respiratory depression over 8 weeks.
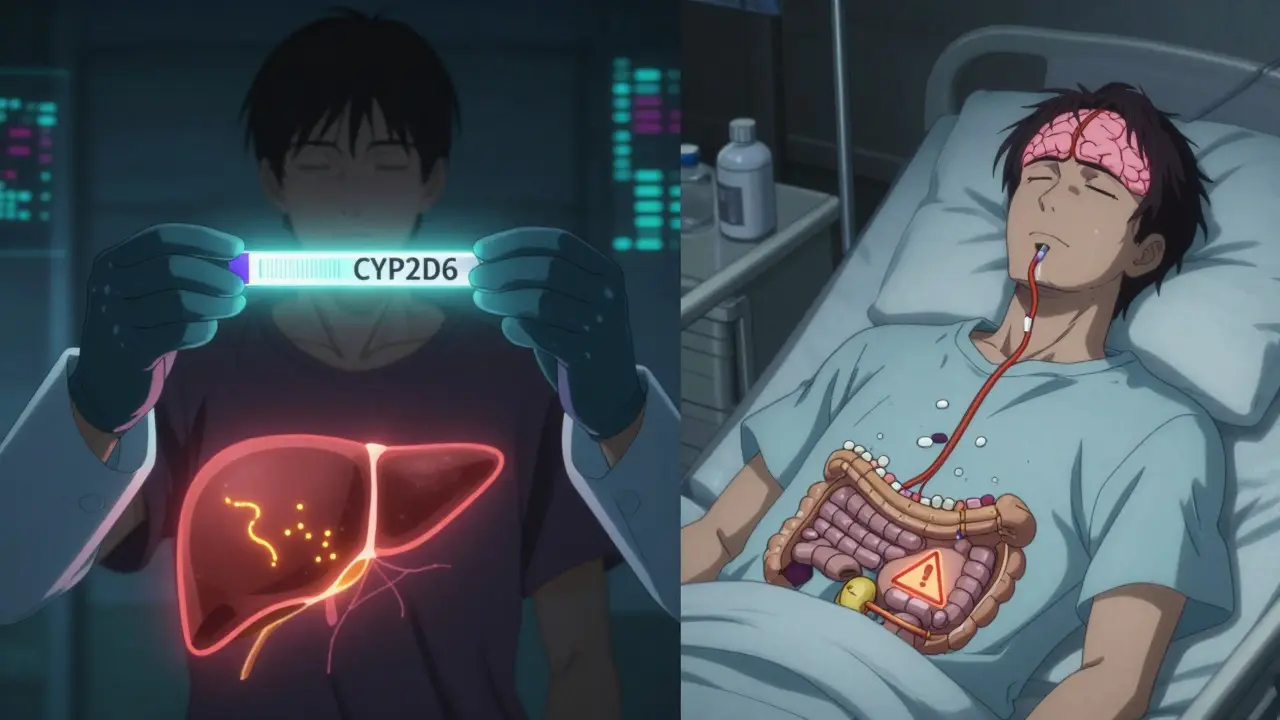
And there’s genetic testing. About 7-10% of Caucasians have a gene variant (CYP2D6) that makes them poor metabolizers of codeine. For them, the drug doesn’t work at all. Others have the opposite-rapid metabolizers who feel strong effects from tiny doses. By 2030, experts predict 40% of pain and mental health prescriptions will be guided by these genetic markers.
What You Can Do Right Now
- Track your side effects. Keep a simple log: date, symptom, severity (1-10). You’ll see patterns.
- Don’t assume fading side effects mean better results. A lack of nausea doesn’t mean the drug is more effective. It just means your body adapted.
- Ask your doctor: “Which side effects will fade, and which won’t?” Most don’t know the answer-but they should.
- Never increase your dose because side effects disappeared. That’s how overdoses happen.
- If a side effect persists, ask about management-not just tolerance. Constipation? Laxatives. Sexual dysfunction? Dose timing or add-ons. Fatigue? Adjust timing or try non-drug strategies.
Tolerance isn’t a flaw. It’s a feature of how your body survives. But without understanding it, you’re flying blind. The goal isn’t to eliminate side effects. It’s to know which ones are temporary-and which ones need real solutions.
Why do some side effects disappear but others don’t?
Different side effects come from different parts of the body and involve different receptors. For example, nausea from opioids is controlled by brainstem receptors that adapt quickly, while constipation comes from gut receptors that barely change. Your body adapts faster to some systems than others-this is called differential tolerance.
Does tolerance mean the medication isn’t working anymore?
Not necessarily. Tolerance often affects side effects more than the intended effect. For example, people on benzodiazepines lose sedation within two weeks but still get anxiety relief. Same with SSRIs-nausea fades, but depression improvement continues. Always check if the main benefit is still there before assuming the drug stopped working.
Can I stop taking my medication if side effects go away?
No. Side effects fading doesn’t mean the drug’s effect on your condition has faded. Stopping abruptly can cause withdrawal or make your original condition worse. Always talk to your doctor before making changes-even if you feel fine.
Is it safe to increase my dose because I don’t feel side effects anymore?
No. Just because nausea or dizziness is gone doesn’t mean your body has built tolerance to the dangerous effects-like slowed breathing or heart rate. Increasing your dose without medical supervision can lead to overdose. Always follow your prescribed dose.
Are some people more likely to develop tolerance than others?
Yes. Genetics play a big role. About 7-10% of Caucasians have a gene variant (CYP2D6) that makes them metabolize certain drugs much faster or slower. This affects how quickly tolerance develops. Age, liver health, and other medications also influence tolerance speed.