Ozempic: What It Is, How It Works, and What You Need to Know
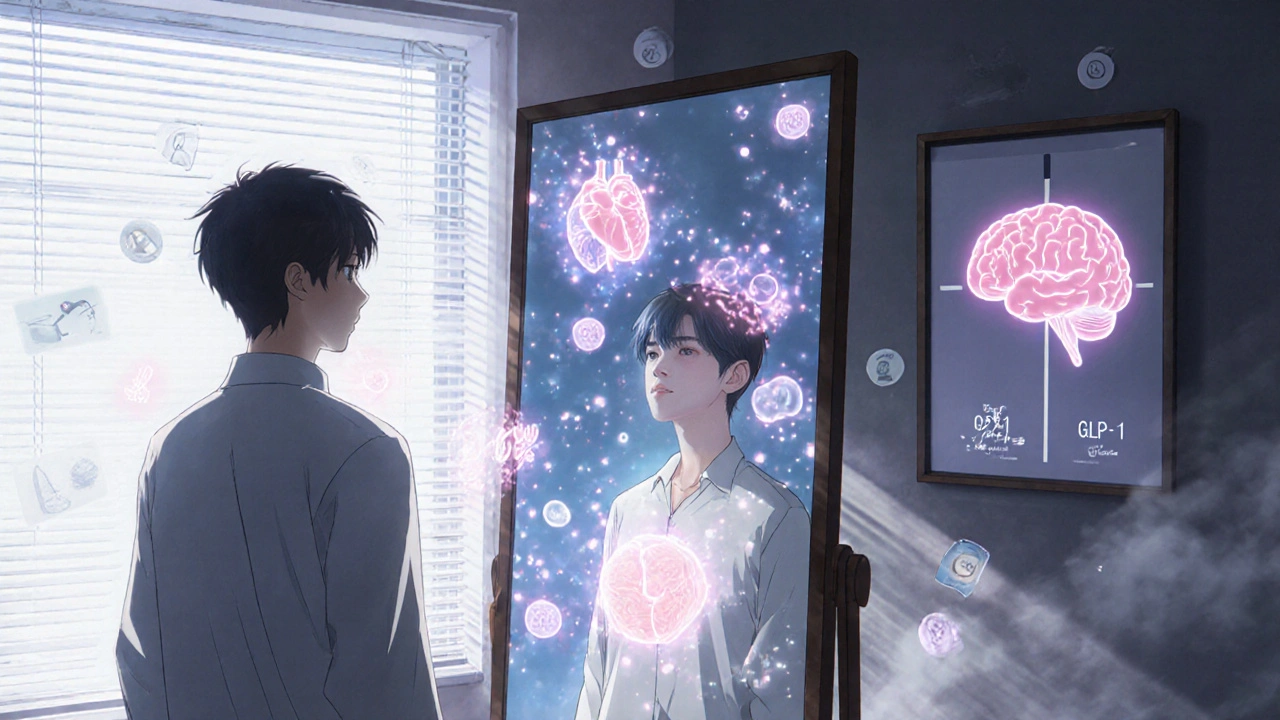
When you hear Ozempic, a once-weekly injectable medication used to treat type 2 diabetes and promote weight loss. Also known as semaglutide, it works by mimicking a natural hormone in your body that helps control blood sugar and appetite. It’s not a magic pill, but for many people, it’s changed how they manage their health—especially when diet and exercise alone aren’t enough.
Ozempic belongs to a class of drugs called GLP-1 agonists. These drugs tell your pancreas to release insulin when blood sugar rises, slow down digestion, and reduce hunger signals to your brain. That’s why people using Ozempic often eat less without feeling deprived. It doesn’t speed up your metabolism—it helps your body make smarter choices about food. Many users report feeling full faster and losing interest in sugary snacks, which is why it’s now commonly used for weight loss, even in people without diabetes. But it’s not for everyone. If you have a personal or family history of thyroid cancer, your doctor won’t prescribe it. And it’s not something you start on a whim—it requires medical supervision and regular check-ins.
People often mix up Ozempic with Wegovy. They’re the same drug—semaglutide—but Wegovy is approved specifically for weight loss and comes in higher doses. Ozempic is FDA-approved for type 2 diabetes, though doctors sometimes prescribe it off-label for weight management. That’s why you’ll see so many stories online about weight loss with Ozempic. But behind those results are real side effects: nausea, vomiting, and stomach discomfort are common at first. Most people adjust after a few weeks. It’s also expensive without insurance, and not all pharmacies stock it reliably. You need to plan ahead.
What you won’t find in ads is how it affects your daily life. Some people feel more energy. Others struggle with fatigue. Some see their blood sugar drop so low they need to carry snacks. Others notice their hair thinning or their skin changing. These aren’t side effects everyone gets—but they’re real enough that you should talk to your doctor before starting. And if you’re thinking about stopping, don’t quit cold turkey. Your blood sugar can spike, and you might regain weight fast. Tapering off under medical guidance matters.
The posts below cover what people actually experience with Ozempic and similar medications. You’ll find guides on managing side effects, how it compares to other weight-loss drugs, what to do if it stops working, and how to talk to your doctor about alternatives. There’s also advice on nutrition, exercise, and mental health while using it. This isn’t about hype. It’s about what works, what doesn’t, and how to stay safe while using it.
GLP-1 Agonists and Weight Loss: Real Benefits Beyond Blood Sugar Control
- Date: 20 Nov 2025
- Categories:
- Author: David Griffiths
GLP-1 agonists like semaglutide and tirzepatide help people lose significant weight, reduce heart risk, and improve metabolic health-far beyond just controlling blood sugar. Learn how they work, who benefits most, and what the real costs and side effects are.