Food-Drug Interactions: What You Need to Know Before You Eat or Take Medicine
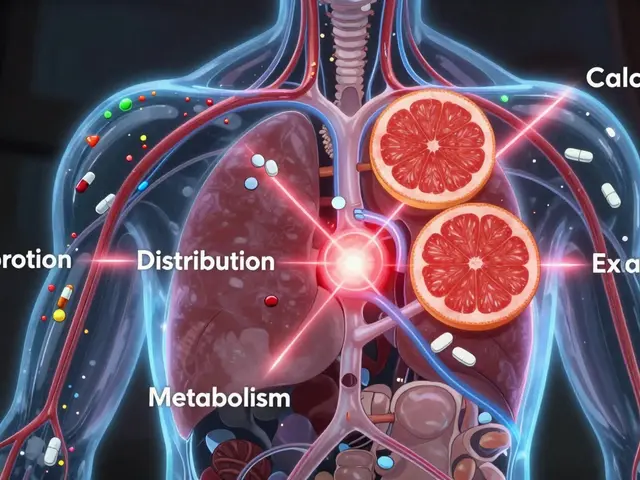
When you take a medication, it doesn’t just interact with your body—it interacts with food-drug interactions, the unintended effects that happen when what you eat or drink changes how a medicine works in your system. Also known as dietary interactions, these can turn a safe treatment into a risk, or make your pill useless. It’s not just about grapefruit and statins. It’s about your morning coffee, your daily vitamin, your glass of wine, even your spinach smoothie.
Take warfarin, a blood thinner often prescribed after heart surgery or for atrial fibrillation. Eat more leafy greens one week, and your blood clots faster. Skip them, and you bleed too easily. Your doctor doesn’t tell you to avoid spinach—they tell you to keep it steady. Same with antibiotics like tetracycline, a common treatment for acne and infections. Take it with milk or calcium supplements? It won’t absorb. You might as well have swallowed a pill-shaped piece of chalk. And then there’s SSRIs like fluoxetine, used for depression and anxiety, which can spike serotonin dangerously if mixed with certain herbal supplements like St. John’s wort. These aren’t rare edge cases. They happen every day.
You don’t need to become a pharmacist, but you do need to know the basics. Some medicines need an empty stomach. Others need food to be absorbed safely. Alcohol can turn painkillers into liver bombs. Grapefruit juice can turn cholesterol meds into overdose risks. Even over-the-counter stuff like antacids or calcium supplements can mess with thyroid pills, iron, or antibiotics. The same goes for dietary supplements, products people take thinking they’re harmless, like magnesium, vitamin K, or green tea extract. Many aren’t tested with prescriptions, but your body doesn’t care—they still react.
That’s why the posts here aren’t just about what to avoid. They’re about what to ask, what to track, and how to talk to your pharmacist without sounding confused. You’ll find real advice on preventing double-dosing, checking labels for hidden ingredients, using pill organizers, and knowing when a supplement is doing more harm than good. You’ll see how EHR systems help pharmacies catch dangerous mixes before you even leave the counter. You’ll learn why mixing steroids and NSAIDs can cause internal bleeding, and how a simple proton pump inhibitor can stop it. This isn’t theory. It’s what happens in kitchens, pharmacies, and hospital rooms every day.
Whether you’re on one pill or five, whether you’re managing diabetes with methotrexate, treating acne with isotretinoin, or just trying to stay healthy with Sandy Everlasting, food-drug interactions don’t care about your intentions. They only care about what’s in your body and when it got there. The good news? You can control it. You just need to know what to look for—and you’re about to find out.
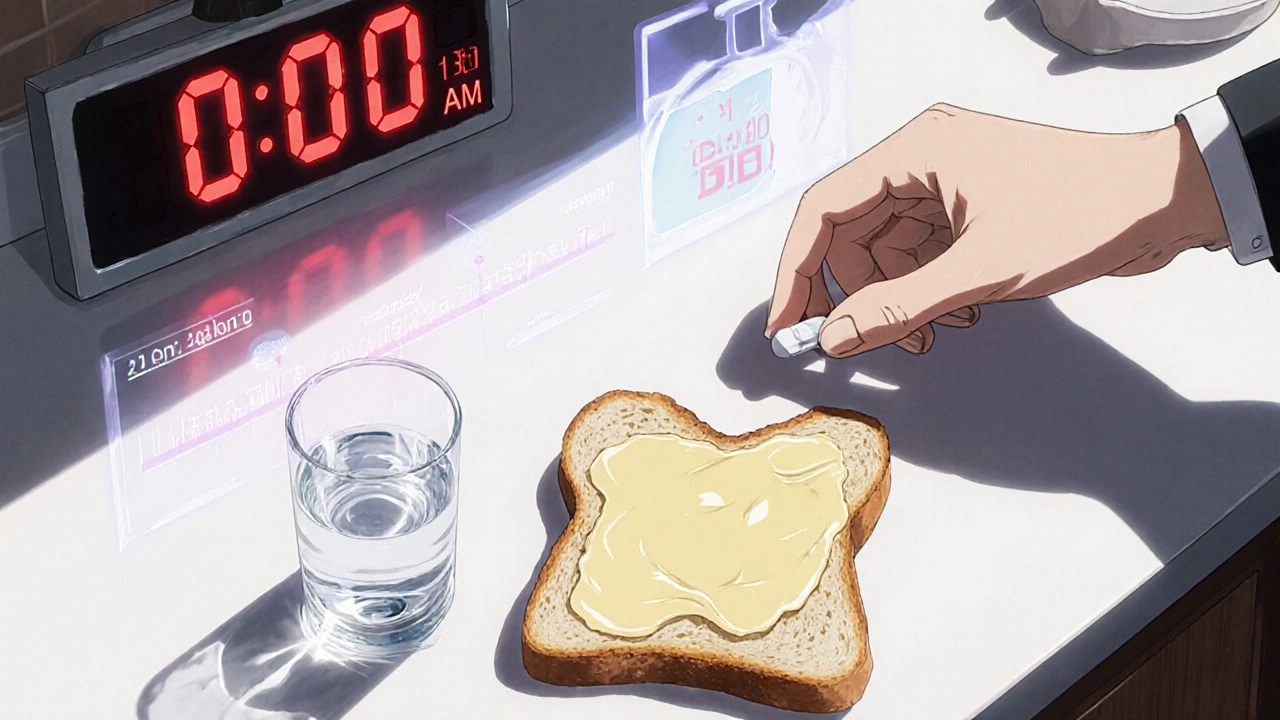
Taking Medications with Food: How Meals Affect Absorption and Timing
- Date: 18 Nov 2025
- Categories:
- Author: David Griffiths
Learn how food affects medication absorption and timing. Discover which drugs need an empty stomach, which need food, and why getting it wrong can reduce effectiveness or cause side effects.