Fertility Medication: Options, Risks, and How They Work
When navigating Fertility Medication, the class of drugs that help people conceive by stimulating ovulation, supporting the uterine lining, or correcting hormonal imbalances. Also known as reproductive drugs, it plays a key role in many family‑building plans. Understanding how these medicines interact with Endocrine Disruptors, chemicals that interfere with hormone signaling and the broader field of Assisted Reproductive Technology, procedures like IVF that often rely on medication to succeed can make the difference between a smooth cycle and unexpected side‑effects. The process known as Ovulation Induction, using drugs such as clomiphene or letrozole to trigger egg release is a core example of how fertility medication is applied in real life.
Key Considerations When Choosing a Fertility Medication
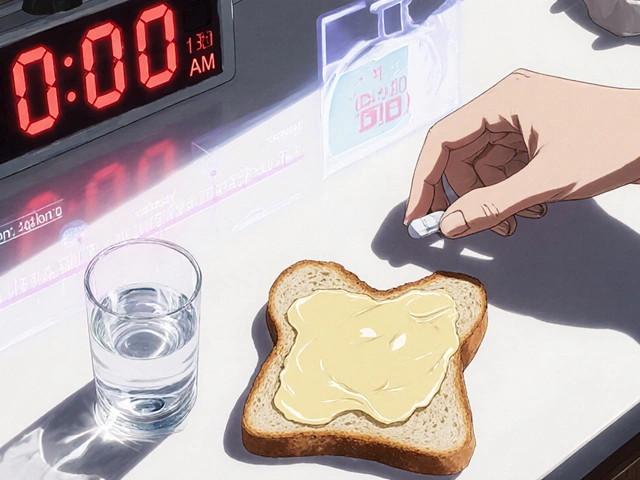
First, know that fertility medication isn’t a single pill; it’s a toolbox. Ovulation inducers like clomiphene citrate and letrozole are often the first line because they’re oral, inexpensive, and work for many women with irregular cycles. If those don’t produce a mature egg, doctors may move to gonadotropins—injectable forms of FSH and LH that directly stimulate the ovaries. While gonadotropins give higher success rates, they also raise the risk of multiple pregnancies and require close ultrasound monitoring. Progesterone support (oral, vaginal, or injectable) is added after egg retrieval or embryo transfer to keep the uterine lining receptive. Finally, aromatase inhibitors such as letrozole reduce estrogen production, which can be useful for patients with polycystic ovary syndrome (PCOS).
These drug classes form a semantic chain: Fertility medication encompasses ovulation induction; ovulation induction requires hormone monitoring; hormone monitoring informs dosage adjustments. The chain shows why a solid partnership with a reproductive endocrinologist matters. The doctor will order baseline blood tests—FSH, LH, estradiol, AMH—and then schedule serial ultrasounds to track follicle growth. Adjustments happen in real time; a slight overshoot can mean a higher chance of twins, while an undershoot might waste a cycle. The interplay between medication and the body’s natural rhythm is what makes each treatment plan unique.
Beyond the drugs themselves, the environment can tip the scales. Studies show that exposure to endocrine disruptors—like bisphenol A in plastics or phthalates in personal care products—can blunt the response to ovulation inducers, forcing higher doses or longer treatment. Reducing these chemicals (choosing glass containers, fragrance‑free soaps, and organic foods) is a simple step that can boost medication effectiveness. Likewise, when patients combine fertility medication with assisted reproductive technology, timing becomes critical. In IVF cycles, for example, the same gonadotropin regimen that works for a fresh embryo transfer may need tweaking for a frozen‑embryo thaw, because the uterine environment has changed. Understanding that fertility medication interacts with both the patient’s internal hormone milieu and external chemical exposures helps set realistic expectations.
Now that you see how the different drug types link together, how monitoring shapes dosing, and how everyday chemicals can interfere, you’re ready to explore the detailed articles below. Each post dives deeper into a specific medication, compares options, or offers practical tips for safe use. Use this overview as a map to find the information that matches your situation, whether you’re just starting to consider medication or fine‑tuning an ongoing cycle.

Clomiphene and Postpartum Depression: Exploring the Possible Link
- Date: 15 Oct 2025
- Categories:
- Author: David Griffiths
Explore how clomiphene's hormonal effects may influence postpartum depression, review research, and get practical advice for managing mood during and after pregnancy.