Epinephrine Auto‑Injector: What You Need to Know
When dealing with epinephrine auto‑injector, a compact, pre‑filled device that delivers a single dose of epinephrine to counter severe allergic reactions. Also known as EpiPen, it is designed for rapid self‑administration or for a caregiver to use in an emergency. The device combines a needle, a spring‑loaded cartridge, and clear dosage instructions so that even a nervous bystander can act confidently.
Severe anaphylaxis can unfold in seconds, and the fastest way to stop airway swelling is a dose of epinephrine delivered by the device. epinephrine auto‑injector provides immediate vasoconstriction, bronchodilation, and heart‑rate support, buying precious minutes until professional care arrives. This emergency tool is essential for anyone with known food, insect, or medication allergies, and many schools and workplaces now keep them on hand.
Common Questions About Using an Auto‑Injector
People often wonder which brand to choose. While EpiPen remains the most recognizable, alternatives like Auvi‑Q offer voice‑guided instructions and a smaller form factor. All approved devices share core attributes: a fixed 0.3 mg or 0.15 mg dose, a safety cap, and an audible click when activated. The choice usually hinges on price, pack size, and personal comfort with the device’s ergonomics.
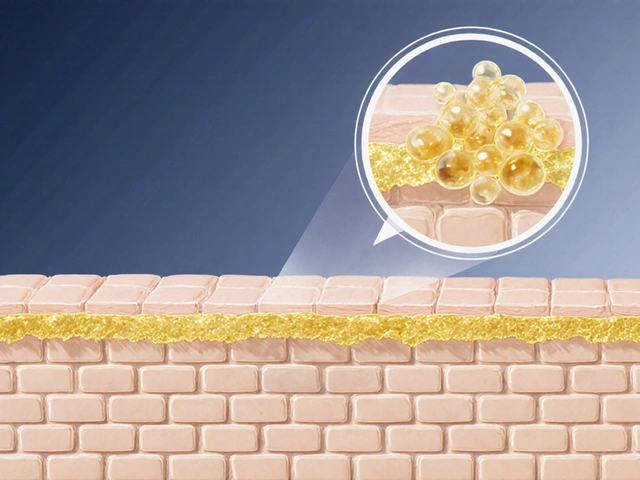
Understanding dosage is another critical piece. Adults and children over 30 kg typically receive 0.3 mg, while smaller children get 0.15 mg. The dosage rule is simple: give the injection into the outer thigh—as far from the mid‑line as possible—and hold the device in place for at least three seconds. This ensures the medication fully absorbs into the muscle tissue.
Training dramatically improves outcomes. Studies show that individuals who practice with trainer pens make fewer errors when a real reaction occurs. Training covers three key steps: recognize anaphylaxis signs, remove the safety cap, and press firmly against the thigh. Re‑training every six months helps maintain muscle memory, reducing hesitation during a crisis.
Storage matters, too. Auto‑injectors should stay at room temperature, away from direct sunlight and extreme heat. The drug degrades after its expiration date, so regular checks are a must. If you travel, carry a spare device in a different bag and label each one with the expiration date to avoid confusion.
Legal and insurance considerations can be surprising. Many health plans cover auto‑injectors without a prior authorization, but the brand may affect co‑pay. Some employers offer free devices as part of workplace safety programs. It’s wise to verify coverage before a reaction occurs, and keep receipts for potential reimbursement.
Beyond personal use, schools are required in many regions to maintain an emergency medication stock list. Teachers and staff should know where the auto‑injector is stored, who’s authorized to administer it, and how to contact emergency services. A clear, written action plan—often called an Anaphylaxis Emergency Action Plan (AEAP)—helps coordinate care between parents, school nurses, and local EMS.
Finally, after using the device, seek professional medical evaluation even if symptoms improve. A second dose may be needed if symptoms persist, and a healthcare provider can monitor for delayed reactions. Keep a log of the incident, including the time of injection, brand used, and any side effects, to share with your doctor for future care planning.
All of these points—recognition, device choice, proper technique, training, storage, and follow‑up—form the backbone of effective anaphylaxis management. Below you’ll find a curated list of articles that dive deeper into each of these topics, from brand comparisons to step‑by‑step usage guides, helping you stay prepared and confident when seconds count.

Food Allergy Guide for Parents: Managing Symptoms, Treatments & Labeling
- Date: 8 Oct 2025
- Categories:
- Author: David Griffiths
A practical guide for parents on spotting food allergy symptoms, creating emergency plans, using epinephrine injectors, reading labels and staying safe.