Chlorpromazine Comparison: Classic Antipsychotic vs Modern Options
When reviewing chlorpromazine, a low‑potency typical antipsychotic introduced in the 1950s. Also known as Thorazine, it blocks dopamine D2 receptors and is used for schizophrenia, bipolar mania, and severe nausea.
How It Stacks Up With Other Antipsychotics
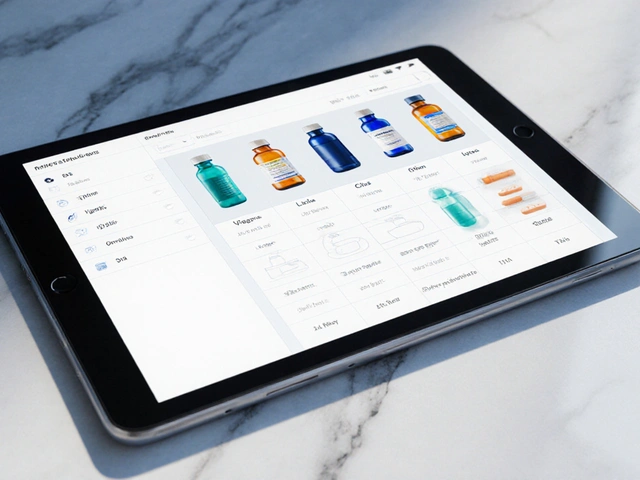
Another well‑known typical drug is haloperidol, a high‑potency antipsychotic famous for its strong D2 blockade. Compared to chlorpromazine, haloperidol delivers quicker symptom control but brings a higher risk of extrapyramidal side‑effects. Moving to atypical agents, risperidone, an atypical antipsychotic that balances dopamine and serotonin antagonism offers mood‑stabilizing benefits and fewer motor issues, yet it can raise prolactin levels. The most distinct alternative is clozapine, the only atypical antipsychotic proven to reduce suicide risk in schizophrenia. Clozapine’s side‑effect profile includes agranulocytosis, demanding regular blood monitoring, which makes it a last‑resort choice despite its superior efficacy for treatment‑resistant cases.
These four agents illustrate three core semantic triples: chlorpromazine comparison encompasses typical antipsychotics; typical antipsychotics require dopamine D2 blockade; atypical antipsychotics influence serotonin pathways. Understanding these relationships helps clinicians match a drug’s potency, side‑effect risk, and therapeutic niche to a patient’s profile. For instance, if a patient struggles with sedation, chlorpromazine’s antihistamine activity may be a drawback, while haloperidol’s leaner profile could be preferable. Conversely, if metabolic concerns dominate, risperidone’s moderate weight gain may be more acceptable than clozapine’s heavier metabolic impact.
Beyond the drugs themselves, other entities shape the comparison landscape. Pharmacogenomics can predict how quickly a patient metabolizes chlorpromazine via CYP2D6, influencing dose adjustments. Formulation type—oral tablets versus intramuscular depot—affects adherence, especially in long‑term maintenance. Lastly, health‑system factors like insurance coverage and monitoring requirements often tip the balance toward a cheaper, low‑monitoring option such as chlorpromazine, even when newer agents might offer clinical advantages.
Below you’ll find a curated set of articles that dive deeper into each of these points. Expect detailed tables of efficacy scores, side‑effect frequency charts, cost‑analysis breakdowns, and real‑world prescribing tips. Whether you’re a clinician fine‑tuning a regimen or a patient curious about why your doctor chose a particular antipsychotic, the collection ahead provides the practical context you need to make an informed decision.

Thorazine (Chlorpromazine) vs Common Antipsychotic Alternatives: Detailed Comparison
- Date: 9 Oct 2025
- Categories:
- Author: David Griffiths
A thorough comparison of Thorazine (chlorpromazine) with common antipsychotic alternatives, covering efficacy, side effects, dosing, and how to choose the right medication.