Steroid-NSAID GI Bleeding Risk Calculator
This calculator estimates your risk of gastrointestinal bleeding when taking both steroids and NSAIDs together. Based on clinical guidelines, the risk increases significantly with multiple risk factors.
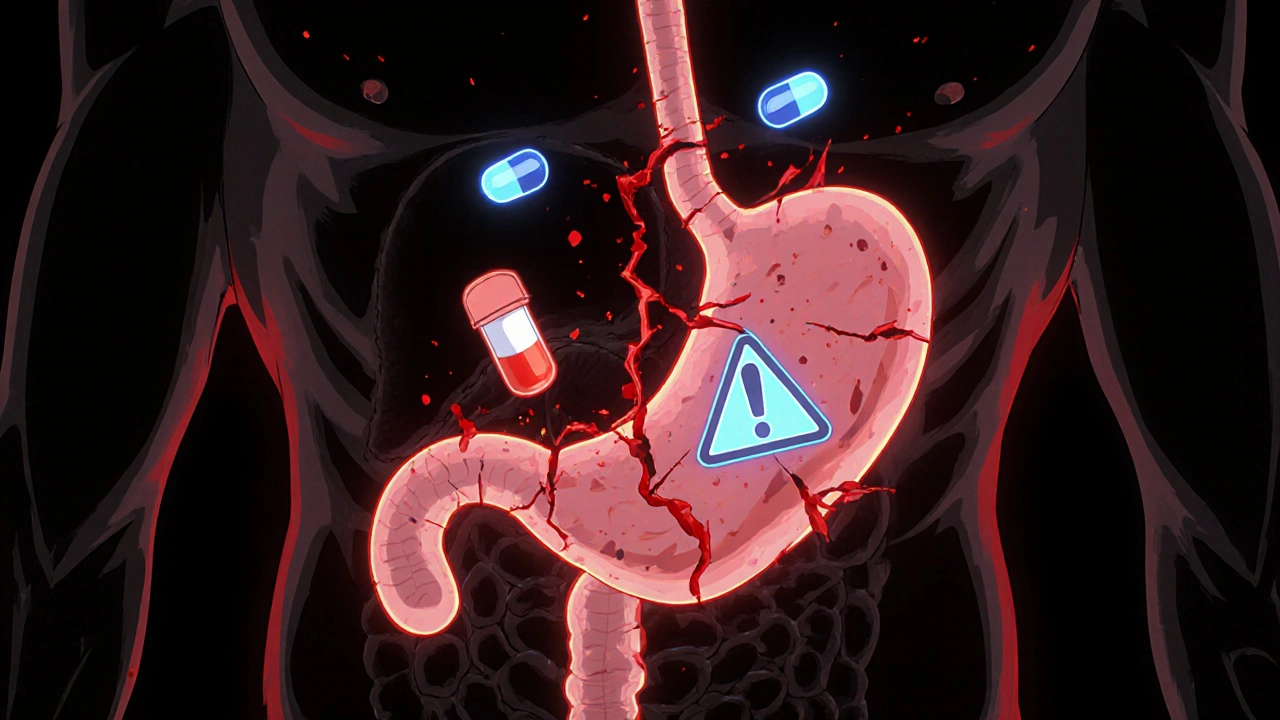
When you take a steroid like prednisone for a flare-up of arthritis or an autoimmune condition, and you’re already on ibuprofen or naproxen for pain, you might think you’re just managing two separate problems. But what you’re really doing is lighting a fuse on your digestive tract. The combination of systemic corticosteroids and NSAIDs doesn’t just add risk-it multiplies it. Studies show this mix can raise your chance of a serious gastrointestinal bleed by nearly 9 times compared to taking neither drug. And most people have no idea.
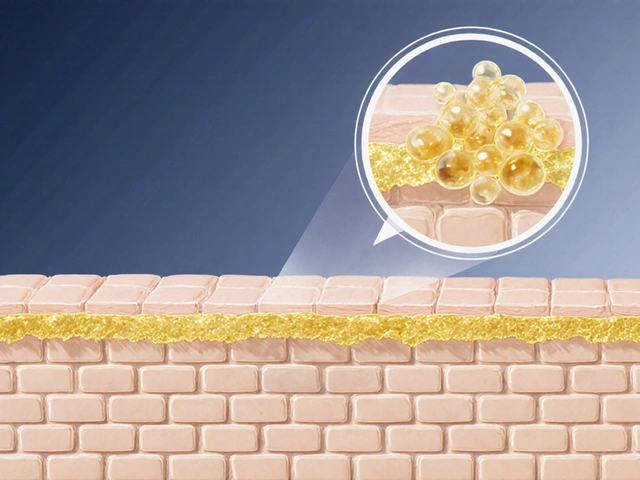
Why This Combo Is So Dangerous
NSAIDs work by blocking enzymes called COX-1 and COX-2. COX-2 is linked to inflammation and pain, which is why these drugs help. But COX-1 is the one that protects your stomach lining. It helps produce prostaglandins-chemicals that keep mucus flowing, blood circulating in the stomach walls, and acid levels in check. When NSAIDs shut down COX-1, your stomach loses its natural shield. That’s why even a single daily dose of ibuprofen can cause ulcers over time. Corticosteroids like prednisone, methylprednisolone, or dexamethasone make this worse in three ways. First, they slow down healing. If a small ulcer starts forming, steroids prevent it from repairing itself. Second, they reduce mucus production, leaving the stomach even more exposed. Third-and this is the sneakiest part-they mask symptoms. You might feel less pain because steroids reduce inflammation, so you don’t realize you’re bleeding internally until it’s too late. The result? A perfect storm. A 2001 study published in the American Journal of Epidemiology found that people taking both drugs had an 8.9 times higher risk of upper GI bleeding or perforation than those taking neither. For those on high-dose NSAIDs (like 1200 mg of ibuprofen daily or more), that risk jumps to over 12 times higher.It’s Not Just Your Stomach
Most people think NSAID-related bleeding means a bleeding ulcer in the stomach or duodenum. But nearly one-third of serious NSAID-related bleeds happen in the lower GI tract-colon, small intestine. A 1999 study found that 86% of patients with lower GI bleeds had taken NSAIDs. And when steroids are added, the risk doesn’t just go up-it spreads. Your entire digestive system becomes vulnerable. This isn’t just a problem for older adults or people with a history of ulcers. Even short-term steroid bursts-like a 5-day prednisone pack for a sinus infection-can trigger bleeding if you’re also taking daily NSAIDs. A 2019 study showed the risk rises within just 7 days of starting the combo. That means if you’re on a weekend trip and take ibuprofen for a headache, then get prescribed prednisone for a cough, you’re already in danger.Not All NSAIDs Are Created Equal
Some NSAIDs are far worse than others. Traditional NSAIDs like naproxen, diclofenac, and high-dose ibuprofen are the biggest culprits. They strongly block COX-1, which is why they’re more likely to cause bleeding. In contrast, COX-2 inhibitors like celecoxib (Celebrex) were designed to spare COX-1. Studies show they cut upper GI bleeding risk by about half compared to traditional NSAIDs. But here’s the catch: even celecoxib isn’t safe with steroids. The risk is lower, but still elevated. A 2017 trial called CONCERN found that for patients on both aspirin and NSAIDs, celecoxib plus a PPI reduced bleeding risk by 54% compared to naproxen plus PPI. That’s a big win-but only if you’re taking the PPI. Without it, celecoxib with steroids still carries a dangerous risk.Who’s at Highest Risk?
You’re in the danger zone if you have even one of these:- Age 65 or older
- History of peptic ulcer or GI bleeding
- Taking blood thinners like warfarin, apixaban, or rivaroxaban
- Using multiple NSAIDs (e.g., ibuprofen + aspirin)
- On high-dose NSAIDs (ibuprofen ≥1200 mg/day, diclofenac ≥100 mg/day)
- Using systemic steroids for more than 7 days
- Diagnosed with heart disease, kidney disease, or liver disease

What Actually Works: PPIs Are the Gold Standard
The only proven way to prevent this kind of bleeding is with a proton pump inhibitor (PPI). That’s drugs like omeprazole, esomeprazole, pantoprazole, or lansoprazole. They work by shutting down stomach acid production at the source. Less acid means less irritation to damaged tissue, giving your stomach time to heal. PPIs are far better than H2 blockers like famotidine (Pepcid) or ranitidine (Zantac). A 2020 review found PPIs reduce NSAID-induced ulcers by 73%, while H2 blockers only cut risk by 48%. That’s a huge difference. And PPIs work even when steroids are involved. For low-risk patients: one daily dose of omeprazole 20 mg is enough. For high-risk patients: double the dose-omeprazole 40 mg daily-is recommended. This is especially true if you’re on anticoagulants or have a past ulcer.The Stark Reality: Most Doctors Don’t Prescribe It
Here’s the scary part: even though guidelines have been clear since 2021, most doctors still don’t act on them. A 2022 study of over 12,000 hospital patients found that only 38.7% of those on both NSAIDs and steroids got a PPI. In non-rheumatology clinics? Just 22.3%. Why? Because many clinicians still think:- “It’s just a short steroid course-it won’t hurt.”
- “The patient says they’re fine.”
- “They’re on OTC ibuprofen, so it’s not a big deal.”
What You Can Do Right Now
If you’re currently taking both a steroid and an NSAID:- Stop taking NSAIDs if possible. Ask your doctor if acetaminophen (paracetamol) can manage your pain instead. It doesn’t affect the stomach lining.
- If you must keep the NSAID, ask for a PPI. Don’t wait for your doctor to bring it up. Say: “I’m on prednisone and ibuprofen. Am I at risk for bleeding? Should I be on a PPI?”
- Don’t switch to H2 blockers. Famotidine or ranitidine won’t protect you enough.
- Watch for warning signs. Black, tarry stools; vomiting blood or material that looks like coffee grounds; sudden dizziness or fainting; severe abdominal pain. These are emergencies. Go to the ER.
- Check your OTC meds. Many cold and flu pills contain NSAIDs like ibuprofen or naproxen. Read labels.
New Hope: Combination Drugs and Genetic Testing
There’s good news on the horizon. In 2023, the FDA approved a new pill called Vimovo, which combines naproxen with esomeprazole in one tablet. Clinical trials showed it cut endoscopic ulcers by 54% compared to naproxen alone. It’s designed for high-risk patients who need NSAIDs but can’t avoid them. Researchers are also looking at genetics. Some people have variations in the CYP2C9 and PTGS1 genes that make them much more likely to develop GI bleeding from NSAIDs. Early data suggests these genetic differences can increase risk by over 2 times. In the future, a simple blood test might tell you if you’re genetically vulnerable-before you even start the drugs.What the Experts Are Saying
Dr. Colin W. Howden, past president of the American College of Gastroenterology, calls this combination “one of the most dangerous yet underappreciated drug interactions in clinical practice.” He’s right. We’ve known about this for over 20 years. We have clear guidelines. We have effective, cheap, safe drugs to prevent it. Yet it keeps happening. Because prevention requires action-not just knowledge. And action means asking the right questions, pushing for protection, and refusing to accept “it’s probably fine” as an answer. The Mayo Clinic cut bleeding events by nearly 70% by automatically prescribing PPIs whenever a steroid and NSAID are ordered together. That’s not magic. That’s system design. It’s time for every clinic, hospital, and pharmacy to do the same.Bottom Line
Steroids and NSAIDs together are not a harmless combo. They’re a ticking time bomb for your gut. The risk is real, well-documented, and preventable. If you’re on both, you’re not being careful-you’re being lucky. And luck runs out. The solution isn’t complicated: if you’re taking steroids and NSAIDs, you need a PPI. No exceptions. No excuses. No waiting for symptoms. Your stomach doesn’t warn you before it bleeds. But you can still protect it.Can I take ibuprofen with prednisone if I’m only using it for a few days?
Even short-term use-like a 5-day prednisone burst-combined with daily ibuprofen can significantly raise your risk of gastrointestinal bleeding. Studies show the danger starts within 7 days. If you need pain relief while on steroids, switch to acetaminophen (paracetamol) instead. If you must use ibuprofen, ask your doctor for a proton pump inhibitor (PPI) like omeprazole at the same time.
Are COX-2 inhibitors like celecoxib safer with steroids?
Yes, celecoxib carries about half the risk of upper GI bleeding compared to traditional NSAIDs like naproxen or diclofenac. But it’s not risk-free when combined with steroids. The risk is lower, but still elevated. Always use a proton pump inhibitor (PPI) with any NSAID if you’re also taking steroids-even COX-2 inhibitors.
Can I use famotidine (Pepcid) instead of a PPI to protect my stomach?
No. H2 blockers like famotidine or ranitidine are much less effective than proton pump inhibitors (PPIs) at preventing NSAID- and steroid-induced ulcers. Studies show PPIs reduce ulcer risk by 73%, while H2 blockers only cut it by 48%. For this combination, PPIs are the only recommended option.
What are the signs of a GI bleed from steroids and NSAIDs?
Watch for black, tarry stools; vomiting blood or material that looks like coffee grounds; sudden dizziness, fainting, or weakness; or severe abdominal pain. These are signs of active bleeding and require immediate medical attention. Don’t wait for pain-steroids can mask it.
Is it safe to take NSAIDs if I’ve had a stomach ulcer before?
No. If you have a history of peptic ulcer or GI bleeding, combining NSAIDs with steroids is extremely dangerous and can lead to life-threatening bleeding. Avoid NSAIDs entirely if possible. If pain relief is essential, use acetaminophen and always pair it with a PPI under medical supervision. Never take NSAIDs with steroids without a PPI if you have a prior ulcer.
How long should I stay on a PPI if I’m taking steroids and NSAIDs?
You should take the PPI for the entire duration that you’re on both the steroid and the NSAID. Don’t stop it just because the steroid course ends-wait until you’ve finished the NSAID too. Some patients need PPIs long-term if they require ongoing pain management. Always follow your doctor’s advice on duration.
Are there any new medications that combine NSAIDs and stomach protection?
Yes. In 2023, the FDA approved Vimovo, a single pill that combines naproxen with esomeprazole (a PPI). It’s designed for high-risk patients who need NSAIDs but can’t avoid them. Clinical trials showed it reduces stomach ulcers by 54% compared to naproxen alone. It’s not a cure-all, but it’s a major step forward for safer pain management.



Just had my doc prescribe prednisone for a flare-up and I was already on ibuprofen for back pain. Never knew this combo was a ticking time bomb. I asked for a PPI right away-no debate. If you're on both, you're playing Russian roulette with your gut. Don't be that guy.