SSRI Side Effect Comparison Tool
Which SSRI is Right for You?
Select the SSRIs you're considering to compare their side effect profiles. This tool helps you understand the common side effects based on the latest research and patient reports.
Key Side Effect Information
Common Mild Side Effects
Most people experience these side effects in the first 7-14 days. They typically fade by week 4-6:
- Nausea (affects ~50% of users)
- Diarrhea or constipation
- Drowsiness or insomnia
- Headaches
- Dry mouth
Most Common & Persistent Side Effect
Sexual dysfunction affects 56% of users and can last longer than 6 months for many people:
- Decreased libido
- Difficulty with erection
- Delayed or absent orgasm
- Reduced sexual pleasure
Side Effect Comparison Results
| Side Effect | Citalopram | Fluoxetine | Sertraline | Escitalopram | Paroxetine | Fluvoxamine |
|---|---|---|---|---|---|---|
| Nausea | 25-30% | 30-35% | 35-40% | 30-35% | 40-45% | 45-50% |
| Sexual Dysfunction | 35-40% | 40-45% | 45-50% | 40-45% | 55-65% | 60-65% |
| Weight Gain | 20-25% | 25-30% (late) | 25-30% | 20-25% | 35-40% | 30-35% |
| Insomnia | 15-20% | 30-35% | 20-25% | 25-30% | 20-25% | 25-30% |
| Discontinuation Syndrome | Low risk | Low risk | Medium risk | Medium risk | High risk | Very high risk |
| QT Prolongation Risk | High at high doses | Low | Low | Low | Low | Low |
How to Choose the Right SSRI
For Most Tolerable Side Effects
Citalopram has the highest tolerability rating (1) and lowest risk of severe side effects. It's often the first choice for new patients.
For Anxiety Disorders
Sertraline and Escitalopram are most effective for anxiety and have a good balance of efficacy and tolerability.
- Side effect experiences vary greatly between individuals
- Sexual side effects are the most common reason people stop taking SSRIs
- Weight gain is most common with Paroxetine and Fluvoxamine
- Never stop taking SSRIs abruptly
- Always consult with your doctor before making changes to your medication
When you start taking an SSRI for depression or anxiety, you’re not just hoping for better moods-you’re also signing up for a list of possible side effects. Some are mild and fade quickly. Others stick around, change your life, or even scare you. The truth? Almost 9 out of 10 people on SSRIs experience at least one side effect. And for more than half, those side effects are bad enough to make them question whether the medication is worth it.
What Are SSRIs, Really?
SSRIs stand for Selective Serotonin Reuptake Inhibitors. They’re not magic pills. They work by blocking the brain from reabsorbing serotonin, a chemical that helps regulate mood, sleep, and even digestion. More serotonin in the space between nerve cells means better signaling-and for many people, that means less sadness, less panic, less overwhelm. The first SSRI, fluoxetine (Prozac), hit the market in 1987. It was a game-changer because older antidepressants like tricyclics had brutal side effects: dry mouth, blurry vision, heart rhythm problems, even overdose risks. SSRIs were safer, easier to tolerate, and became the go-to treatment. Today, they make up over 40% of all antidepressant prescriptions in the U.S. Sertraline (Zoloft), escitalopram (Lexapro), and fluoxetine (Prozac) are the most prescribed. But safety doesn’t mean no side effects. It just means the side effects are different-and sometimes, just as troubling.Mild Side Effects: The Common Ones You’ll Likely Experience
Most people on SSRIs get hit with mild side effects in the first few weeks. These aren’t dangerous, but they’re annoying enough to make you wonder if you made the right choice.- Nausea: About half of users feel sick to their stomach, especially right after taking the pill. It’s worse on an empty stomach. Taking the medication with food cuts this down by 60%.
- Diarrhea or constipation: Your gut is full of serotonin receptors. When SSRIs flood the system, digestion gets messy. Diarrhea is more common early on; constipation can show up later.
- Drowsiness or insomnia: Some SSRIs make you sleepy (like paroxetine), others keep you awake (like fluoxetine). Timing matters-taking it in the morning helps avoid sleep issues.
- Headaches: Often tied to serotonin spikes in the brain. Usually fades after two weeks.
- Dry mouth: A classic side effect. Chewing sugar-free gum or sipping water helps.
- Dizziness or lightheadedness: Especially when standing up fast. Slow movements help.
Sexual Dysfunction: The Most Common and Most Damaging Side Effect
If you ask people why they quit SSRIs, sexual side effects will come up again and again.- Decreased libido (sex drive)
- Difficulty getting or keeping an erection
- Delayed or absent orgasm
- Reduced sexual pleasure
- Dose reduction: Lowering the dose helps in 40% of cases.
- Switching SSRIs: Bupropion (Wellbutrin) is often added because it doesn’t cause sexual side effects. Some doctors prescribe it alongside an SSRI.
- Medication holidays: Skipping doses on weekends (under doctor supervision) helps some, but isn’t safe for everyone.
- PDE5 inhibitors: Drugs like sildenafil (Viagra) improved sexual function in 67% of men in a clinical trial.
Weight Gain: It’s Not Just in Your Head
People assume weight gain on SSRIs is from eating more because they feel better. Sometimes, yes. But often, it’s the drug itself.- 49% of users report weight gain.
- Paroxetine and mirtazapine (not an SSRI, but often compared) are the worst offenders.
- Fluoxetine tends to cause weight loss early on, then weight gain later.
Severe Side Effects: When to Get Help Immediately
Most side effects fade. But some need urgent attention.Serotonin Syndrome
This is rare-but deadly. It happens when serotonin builds up too much, usually when SSRIs are mixed with other drugs like tramadol, MDMA, certain migraine meds, or even St. John’s Wort. Symptoms start mild:- Rapid heartbeat
- Sweating
- Tremors
- Agitation
- High fever
- Muscle rigidity
- Confusion
- Seizures
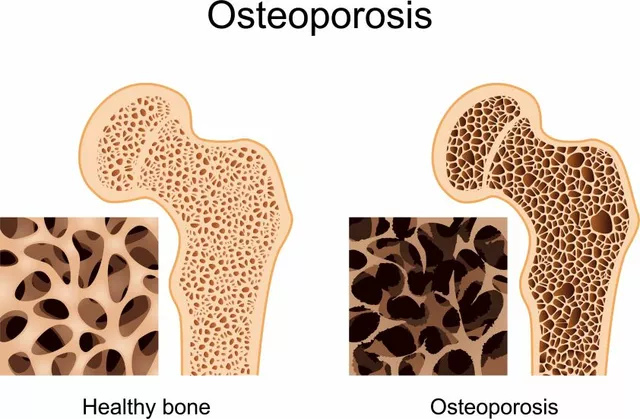
Hyponatremia (Low Sodium)
SSRIs are the #1 antidepressant class linked to dangerously low sodium levels, especially in older adults. Risk factors:- Age over 65
- Female gender
- Low body weight
- Already taking diuretics or other drugs that lower sodium
- Nausea
- Headache
- Confusion
- Seizures or coma in severe cases
Extrapyramidal Symptoms (EPS)
These are movement disorders caused by SSRI effects on dopamine pathways.- Akathisia: A feeling of inner restlessness-you can’t sit still.
- Dystonia: Involuntary muscle spasms, often in the neck or eyes.
- Parkinsonism: Tremors, stiffness, slow movement.
Serious Skin Reactions
Very rare, but life-threatening:- Stevens-Johnson Syndrome
- Toxic Epidermal Necrolysis
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)
Discontinuation Syndrome: Quitting Too Fast Can Backfire
You feel better. You want to stop. But if you quit suddenly, your body rebels. This is called SSRI discontinuation syndrome. It’s not addiction. It’s your nervous system adjusting to the sudden drop in serotonin. Symptoms:- Dizziness
- Nausea
- Flu-like symptoms
- Brain zaps (electric shock sensations)
- Anxiety, irritability
- Reduce dose by 10-25% every 2-4 weeks.
- Use liquid formulations or pill splitters for precise cuts.
- Don’t skip days. Consistency matters.
Long-Term Risks: Metabolic Changes and Hidden Costs
SSRIs aren’t just mood drugs. They affect your whole body. Research now shows long-term use increases the risk of:- Insulin resistance
- Type 2 diabetes
- Weight gain that turns into metabolic syndrome
- Annual blood sugar tests
- Cholesterol and triglyceride checks
- Waist circumference measurements
Why Some SSRIs Are Easier to Tolerate Than Others
Not all SSRIs are the same. Here’s how they stack up:| SSRI | Best For | Worst Side Effects | Tolerability Rank |
|---|---|---|---|
| Citalopram (Celexa) | General anxiety, mild depression | QT prolongation (heart rhythm) at high doses | 1 (Best tolerated) |
| Fluoxetine (Prozac) | Long-term use, OCD, bulimia | Insomnia, weight gain later, activation (anxiety early on) | 2 |
| Sertraline (Zoloft) | Depression, PTSD, OCD, panic disorder | Diarrhea, sexual dysfunction | 3 |
| Escitalopram (Lexapro) | Generalized anxiety, depression | Headache, dizziness, memory issues | 4 |
| Paroxetine (Paxil) | Severe anxiety, panic | Weight gain, sexual dysfunction, drowsiness, discontinuation syndrome | 5 |
| Fluvoxamine (Luvox) | OCD, social anxiety | Nausea, dizziness, high discontinuation rate | 6 (Worst tolerated) |

What Patients Are Really Saying
Real stories tell you what the studies don’t. On Reddit’s r/antidepressants, 68% of 1,247 users said sexual dysfunction was their biggest problem. One wrote: “I got better at work, but lost my marriage. I didn’t know the cost.” On Drugs.com, paroxetine has a 4.1/10 rating. The top review says: “I felt like a zombie. No sex drive, gained 30 pounds, couldn’t sleep. I’d rather be sad than feel like this.” Fluoxetine has a 5.4/10. People love it for energy-but hate the insomnia and weight gain. And here’s the kicker: 31% of people quit their first SSRI within three months because side effects were unbearable. Nausea was the #1 reason. Then sexual problems. Then sleep issues.How to Manage Side Effects-Practical Tips
You don’t have to suffer. Here’s what works:- Nausea? Take with food. Ginger tea helps. Avoid greasy meals.
- Insomnia? Take in the morning. Avoid caffeine after noon.
- Sexual issues? Talk to your doctor before assuming it’s permanent. Dose reduction or adding bupropion can help.
- Weight gain? Start a walking routine. Track calories. Don’t wait until you’ve gained 20 pounds.
- Discontinuation symptoms? Never quit cold turkey. Plan your taper with your doctor.
- Brain zaps? They’re scary but harmless. Slowing the taper reduces them.
The Future: Better SSRIs Are Coming
Drug companies aren’t ignoring the problem. A new SSRI called Lu AF35700 is in Phase III trials. Early results show 37% less sexual dysfunction than current SSRIs. Genetic testing is also becoming more common. Some clinics now test for variants in the CYP2D6 and CYP2C19 genes to predict who’s likely to have bad side effects or poor response. And the FDA is pushing for better labeling. All SSRIs now have stronger warnings about metabolic risks and serotonin syndrome. The goal? Not to stop SSRIs-but to use them smarter.Final Thoughts: It’s Not All or Nothing
SSRIs work. For millions, they’re life-saving. But they’re not risk-free. The key isn’t avoiding side effects-it’s managing them. And that starts with knowing what to expect. If you’re starting an SSRI:- Ask your doctor: “Which one has the least side effects for someone like me?”
- Ask: “What should I watch for in the first month?”
- Ask: “What if I can’t handle it?”
- Don’t quit without talking to your doctor.
- Don’t assume it’s your fault.
- Don’t stay silent. Side effects are treatable.
Are SSRI side effects permanent?
Most SSRI side effects fade after a few weeks. But sexual dysfunction and weight gain can persist in some people, even after stopping the medication. This is called Post-SSRI Sexual Dysfunction (PSSD), and while rare, it’s real. If symptoms last beyond 3-6 months after discontinuation, talk to a specialist. There’s no cure yet, but some find relief with time, therapy, or switching to non-SSRI antidepressants like bupropion.
Can I take SSRIs with alcohol?
It’s not recommended. Alcohol can worsen drowsiness, dizziness, and depression. It also increases the risk of serotonin syndrome if you’re taking other medications. Even moderate drinking can reduce the effectiveness of SSRIs. If you drink, talk to your doctor about safe limits-or consider cutting back while on treatment.
Why do SSRIs make me feel worse at first?
SSRIs boost serotonin immediately, but it takes weeks for your brain to adapt. In the first 1-2 weeks, serotonin surges can increase anxiety, agitation, or even suicidal thoughts-especially in people under 25. That’s why doctors monitor patients closely early on. If you feel worse, don’t stop. Call your doctor. They may adjust your dose or add a short-term anti-anxiety medication to help you through the transition.
Do SSRIs cause brain damage?
No. SSRIs do not cause brain damage. They change how brain circuits communicate, but these changes are reversible. Some studies show SSRIs may even promote neuroplasticity-helping the brain form new connections. Claims of brain damage come from misinformation or confusion with other drugs. Long-term use is safe for most people when monitored properly.
What’s the best SSRI for anxiety?
Sertraline (Zoloft) and escitalopram (Lexapro) are the most studied and recommended for anxiety disorders like GAD, panic disorder, and social anxiety. They’re effective, well-tolerated, and have fewer sedating effects than paroxetine. Fluoxetine can work too, but its long half-life makes it harder to adjust if side effects occur. Always start low and go slow.
Can SSRIs cause suicidal thoughts?
In rare cases, especially in people under 25, SSRIs can increase suicidal thoughts in the first few weeks of treatment. This doesn’t mean they cause suicide-it means the brain is adjusting. The risk is highest in the first 1-2 weeks. That’s why doctors monitor young patients closely. If you or someone you know has new or worsening suicidal thoughts, contact a doctor immediately. Never stop SSRIs suddenly without medical guidance.
How long do I need to take SSRIs?
For a first episode of depression, guidelines recommend staying on SSRIs for at least 6-12 months after symptoms improve. For recurrent depression or anxiety, many people stay on them for years. Stopping too soon increases relapse risk by 50-80%. If you want to stop, work with your doctor on a slow taper. Don’t quit just because you feel better-your brain needs time to stabilize.
Are SSRIs addictive?
No. SSRIs are not addictive. You won’t crave them or get high from them. But your body can become physically dependent, meaning stopping suddenly causes withdrawal symptoms (discontinuation syndrome). That’s not addiction-it’s a physiological adjustment. Always taper under medical supervision to avoid this.




SSRIs are pharmacologically elegant but biologically crude. The 5-HT reuptake inhibition mechanism is a blunt instrument applied to a highly nuanced neurochemical landscape. The side effect profile isn't incidental-it's mechanistically inevitable given serotonin's pleiotropic roles in GI motility, sexual function, thermoregulation, and metabolic signaling. The data here is solid, but what's missing is the pharmacokinetic rationale for why fluoxetine's long half-life reduces discontinuation syndrome while paroxetine's short half-life exacerbates it.