Every night, while you sleep, your body might be under silent stress - not from nightmares or noise, but from something far more dangerous: obstructive sleep apnea. If you snore loudly, wake up gasping, or feel exhausted even after 8 hours in bed, you could be one of the 1 billion adults worldwide with this condition. And what most people don’t realize is that this isn’t just a sleep problem - it’s a heart problem in disguise.
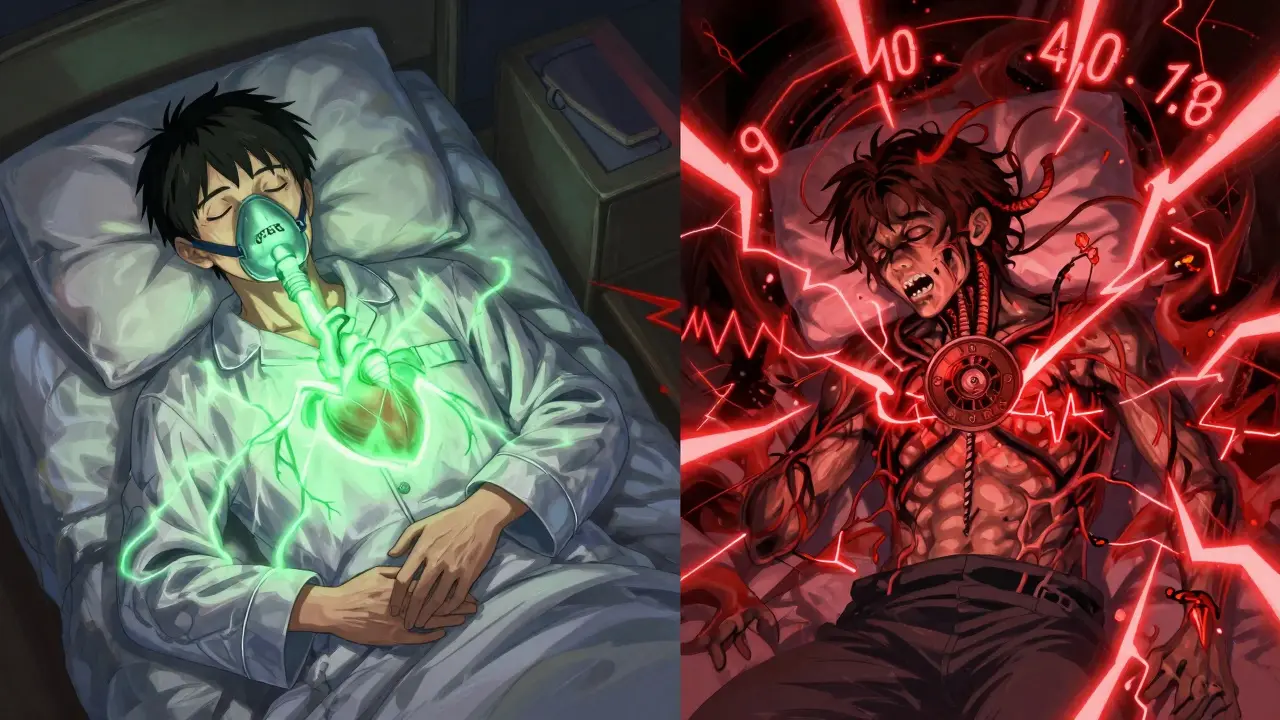
How Sleep Apnea Strains Your Heart
When you have obstructive sleep apnea (OSA), your airway collapses repeatedly during sleep. Each time it happens, you stop breathing for 10 seconds or longer. Your brain panics, jolts you awake just enough to take a breath, then you fall back asleep - often without remembering it. This cycle can happen 30, 50, even 100 times a night.
Each pause in breathing drops your oxygen levels. Your body responds by flooding your system with stress hormones. Your heart rate spikes. Your blood pressure surges by 20 to 40 mmHg - higher than what most people experience during a sprint. And here’s the kicker: this doesn’t just happen at night. Over time, these nightly spikes turn into constant daytime hypertension.
Studies show that 30 to 40% of people with high blood pressure have undiagnosed sleep apnea. Even more alarming: if you have resistant hypertension - meaning your blood pressure stays high despite taking three or more medications - your chances of having OSA jump to over 80%. The American Heart Association now lists sleep apnea as a Class I risk factor for heart disease, meaning it’s as dangerous as smoking or obesity.
The Arrhythmia Connection
It’s not just high blood pressure. Sleep apnea is a major trigger for irregular heart rhythms, especially atrial fibrillation (AFib). During each apnea episode, your heart is thrown into chaos. Oxygen drops. Stress hormones surge. The balance between your sympathetic (fight-or-flight) and parasympathetic (rest-and-digest) nervous systems gets wrecked.
Research from UT Southwestern Medical Center found that people with severe sleep apnea are 3 to 5 times more likely to develop AFib than those without it. That’s worse than the risk from diabetes or obesity alone. And once AFib starts, sleep apnea makes it harder to treat. Even after procedures like ablation, patients with untreated OSA are far more likely to have AFib come back.
One study showed that after 12 months of consistent CPAP therapy, AFib recurrence dropped by 42%. That’s not a small improvement - it’s the difference between needing monthly medication and living without it.
Why This Happens: The Science Behind the Damage
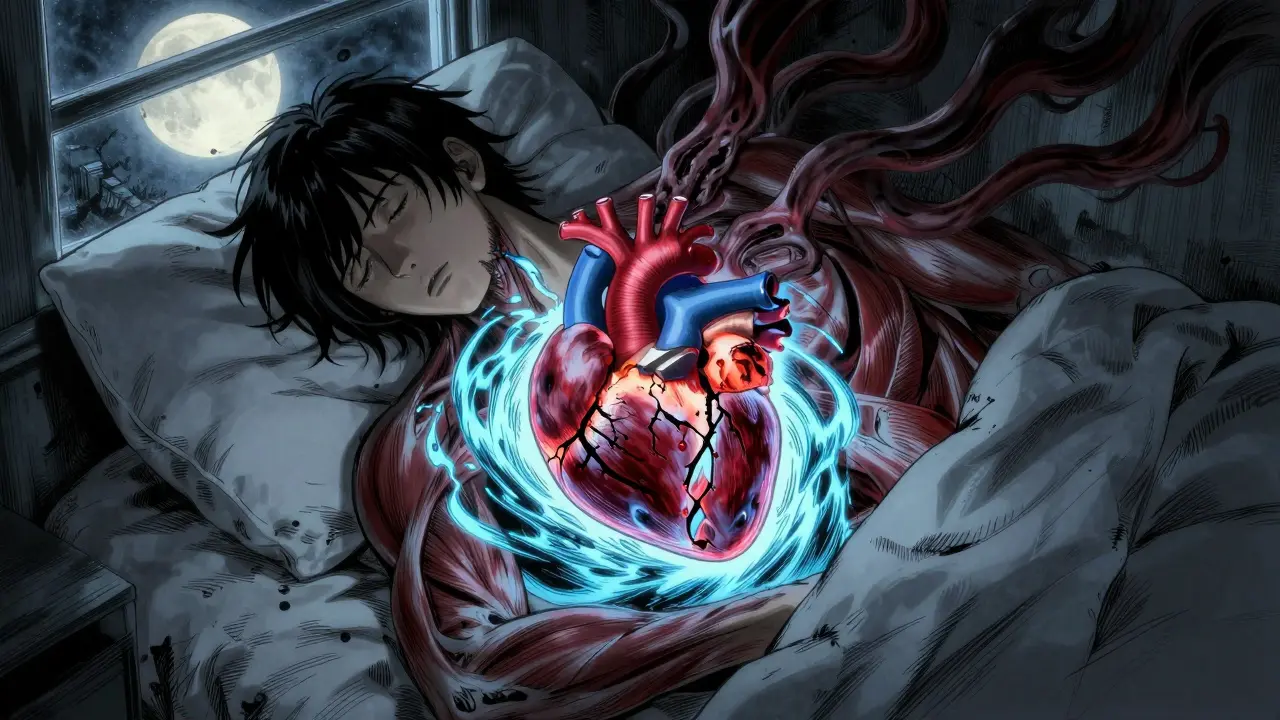
It’s not just about oxygen. Each time your airway closes, your chest creates huge pressure swings - up to -80 cm H2O. That’s like trying to suck air through a straw that’s been pinched shut. Your heart has to work harder to pump blood against that pressure. Over time, this leads to thickening of the heart walls, especially the left ventricle.
By the time most people are diagnosed, 35 to 45% already have diastolic dysfunction - meaning their heart can’t relax properly between beats. This is an early sign of heart failure. Even worse, the repeated oxygen drops cause inflammation and damage to the lining of your blood vessels. Platelets become stickier. Clots form more easily. That’s why people with untreated OSA have a 60% higher risk of stroke and a 30% higher risk of heart attack.
And it’s not just older adults. A 2024 study found that OSA increases heart risk even in people under 40. Younger patients may not have obesity or diabetes, but the mechanical stress on their hearts is just as real.
What You Can Do: Diagnosis and Treatment
If you’re tired all the time, wake up with headaches, or your partner says you snore like a chainsaw, talk to your doctor. Diagnosis is simple: a home sleep test or an overnight sleep study. These tests measure how many times you stop breathing per hour - called the apnea-hypopnea index (AHI). An AHI of 5 or more means you have sleep apnea. Severe cases hit 30 or higher.
The gold standard treatment is CPAP - continuous positive airway pressure. It’s a machine that blows gentle air through a mask to keep your airway open. It’s not glamorous. Some people hate the mask. Others struggle with dry mouth or claustrophobia. But here’s the truth: if you use it 4+ hours a night, 78% report better energy. 65% end up needing fewer blood pressure pills.
One Reddit user, diagnosed with severe OSA (AHI 42), said his blood pressure dropped from 160/95 to 128/82 in just three months after starting CPAP. Another, who had weekly AFib episodes, saw them drop to once every two months after six months of consistent use.
For those who can’t tolerate CPAP, there are alternatives: oral appliances that reposition the jaw, weight loss programs, or newer options like hypoglossal nerve stimulation (Inspire Therapy). These devices work like pacemakers for your airway, stimulating the nerve that controls tongue movement to prevent collapse.
The Hidden Epidemic
Despite all the evidence, only 20 to 25% of at-risk patients are ever screened for sleep apnea in primary care. Doctors focus on cholesterol, blood sugar, and smoking - all important - but rarely ask about snoring or daytime fatigue. Yet, 45 to 65% of people with heart failure, atrial fibrillation, or stroke already have undiagnosed OSA.
That’s why the American Academy of Sleep Medicine now recommends screening for anyone with high blood pressure, AFib, stroke, or heart failure. If you have any of those conditions and haven’t been tested for sleep apnea, you’re missing a critical piece of your heart health puzzle.

What Happens If You Do Nothing?
Untreated sleep apnea doesn’t just make you tired. It slowly breaks your heart. Each night of untreated apnea adds up - like a thousand tiny heart attacks. The longer it goes on, the more damage builds. By the time symptoms like chest pain or shortness of breath appear, the heart may already be permanently changed.
But here’s the good news: unlike genetic risks or aging, sleep apnea is reversible. With treatment, blood pressure drops. Heart rhythms stabilize. The risk of stroke and heart attack goes down. You don’t need to be perfect - just consistent. Even 4 hours of CPAP a night makes a measurable difference.
It’s not about sleeping better. It’s about living longer. Your heart doesn’t rest when you sleep - it’s working harder than ever. If you’re breathing poorly at night, you’re asking your heart to carry a burden it wasn’t meant to hold.
Can sleep apnea cause high blood pressure even if I’m not overweight?
Yes. While obesity increases the risk of sleep apnea, it’s not the only cause. People with narrow airways, large tonsils, or jaw structure issues can have OSA even at a normal weight. The mechanical stress from repeated breathing pauses directly raises blood pressure through sympathetic nervous system activation, regardless of body weight. Studies show that up to 40% of non-obese OSA patients still develop hypertension.
Does treating sleep apnea help with atrial fibrillation?
Absolutely. Treating OSA with CPAP reduces atrial fibrillation recurrence by 42% after one year. It also improves the success rate of procedures like ablation. Untreated sleep apnea causes inflammation and scarring in the atria, making AFib more likely to return. Addressing the root cause - the breathing pauses - helps stabilize your heart’s electrical system.
Is CPAP the only treatment for sleep apnea?
No. CPAP is the most common and effective treatment, but alternatives exist. Oral appliances that shift the jaw forward work well for mild to moderate cases. Weight loss can eliminate OSA in many people. For those who can’t tolerate CPAP, hypoglossal nerve stimulation (like Inspire Therapy) is a surgical option that has shown a 79% reduction in breathing pauses. Positional therapy (sleeping on your side) also helps some patients.
How long does it take for CPAP to lower blood pressure?
Most people see a drop in blood pressure within 2 to 4 weeks of consistent use. On average, systolic pressure drops by 5 to 10 mmHg. The biggest improvements happen in those who use CPAP for at least 4 hours per night. The effect is strongest in people with resistant hypertension and severe OSA (AHI over 30).
Should I get tested for sleep apnea if I have heart disease?
Yes - especially if you have high blood pressure, atrial fibrillation, heart failure, or have had a stroke. Between 45% and 65% of people with these conditions have undiagnosed sleep apnea. Screening is simple and covered by Medicare and most insurance plans. Finding and treating OSA can reduce your risk of future heart events and improve your response to other treatments.
Next Steps: What to Do Today
If you suspect you have sleep apnea, don’t wait. Talk to your doctor about a sleep study. Ask if your blood pressure or heart rhythm issues could be linked to breathing problems during sleep. Bring up snoring, daytime fatigue, or waking up gasping. These aren’t minor complaints - they’re warning signs.
If you’ve been diagnosed and are struggling with CPAP, don’t give up. Try different masks. Use humidification. Adjust the ramp setting. Most people adapt within a month. And remember - every hour of use counts. Even partial improvement reduces your heart risk.
Your heart doesn’t get a day off. If your breathing stops at night, it’s working overtime. Fix the breathing - and you might just save your heart.




i snore like a chainsaw too and wake up exhausted. never thought it was my heart. guess i’m getting tested tomorrow.