If you have allergies and keep getting sinus infections, you’re not alone. Millions of people with hay fever or dust mite allergies end up with persistent sinus inflammation that won’t go away, no matter how many decongestants they try. The problem isn’t just a cold that lingers-it’s your immune system stuck in overdrive, reacting to allergens and turning your sinuses into a constant battleground. Treating this isn’t about popping antibiotics every time your nose feels stuffed. It’s about breaking the cycle between allergies and sinusitis, and knowing exactly when to call in a specialist.
Why Allergies and Sinusitis Go Together
Allergies don’t just make you sneeze. They cause swelling in the nasal passages, which blocks the tiny channels that drain your sinuses. When mucus can’t flow out, it gets trapped, creating the perfect environment for bacteria to grow. That’s when a simple allergic flare-up turns into bacterial sinusitis. But here’s the twist: even without infection, the swelling and inflammation from allergies alone can feel like a sinus infection-pressure behind your eyes, thick mucus, headaches, and fatigue. This is called allergic sinusitis, and it’s not always caused by germs. Studies show that up to 70% of acute sinusitis cases clear up on their own. But for people with allergies, the recurrence rate is much higher. Why? Because the triggers-pollen, mold, pet dander-are still in the air. Unless you stop the allergic response, the inflammation keeps coming back. And over time, that constant swelling can lead to nasal polyps, which are soft, noncancerous growths that block your sinuses even more. In fact, about 30-40% of all chronic sinusitis cases are tied directly to allergic triggers.First-Line Treatments That Actually Work
The best place to start isn’t with antibiotics. It’s with two proven, non-drug approaches: nasal corticosteroids and saline irrigation. Nasal sprays like fluticasone (Flonase), mometasone (Nasonex), and budesonide (Rhinocort) reduce inflammation right where it’s happening. They’re not instant fixes-you need to use them daily for 2 to 4 weeks before you feel real relief. Many people stop after a few days because they don’t see results fast enough. But if you stick with it, studies show these sprays reduce symptoms by about 65%. That’s far better than oral antihistamines like cetirizine, which only help about 42% of the time. Saline irrigation is just as important. Using a neti pot or squeeze bottle with distilled or boiled water and a saline packet helps flush out allergens, mucus, and irritants. Do it once or twice a day. The key is using the right water. Tap water can carry dangerous microbes like Naegleria fowleri, which has caused rare but deadly brain infections. Always use sterile water. People who do this consistently report fewer infections and less need for medication.When Antibiotics Are (and Aren’t) Helpful
Antibiotics like amoxicillin are often prescribed for sinus infections, but they’re only useful in about 1 in 5 cases among allergy sufferers. Why? Because most of the time, the problem isn’t bacteria-it’s inflammation from allergies. Studies show antibiotics alone work in only 35-45% of allergy-related sinusitis cases, compared to 78-87% in pure bacterial infections. The American Academy of Family Physicians says antibiotics should only be used if symptoms last more than 10 days, get worse after improving, or are severe from the start (like high fever or facial swelling). Even then, they’re a temporary fix. If your allergies aren’t controlled, the infection will come back. Antibiotics also contribute to resistance, making future infections harder to treat.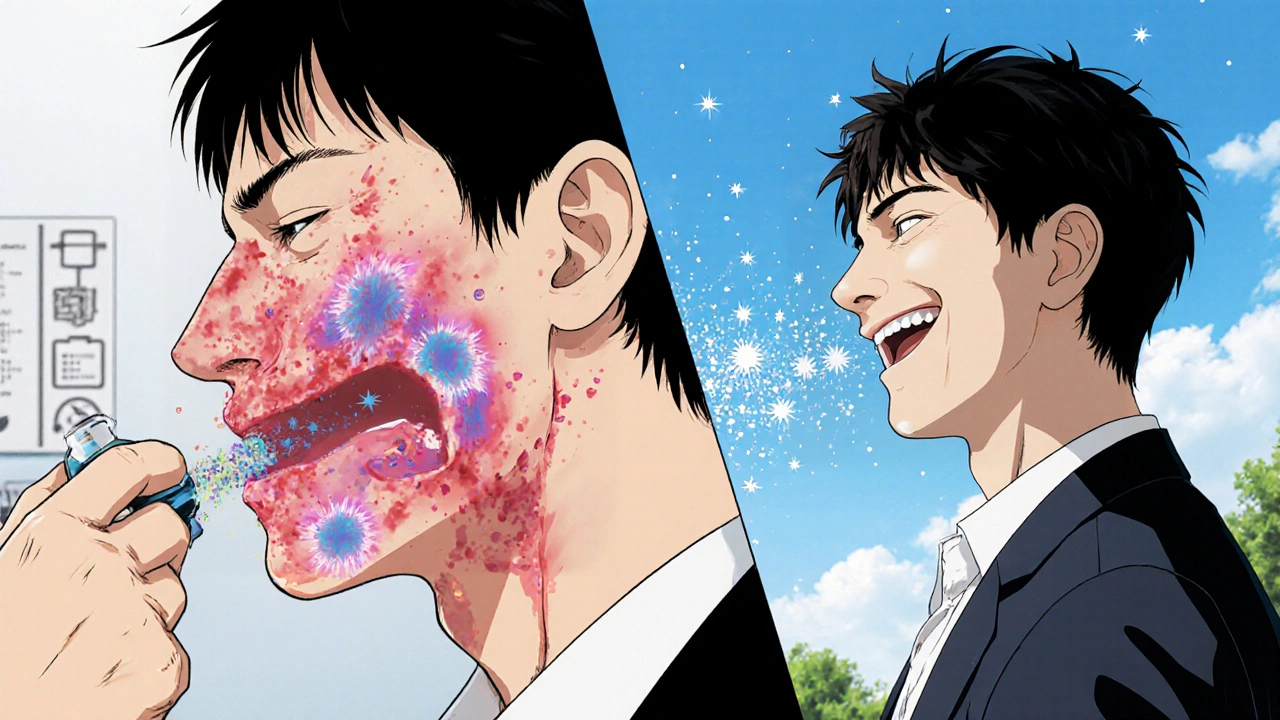
Advanced Options for Stubborn Cases
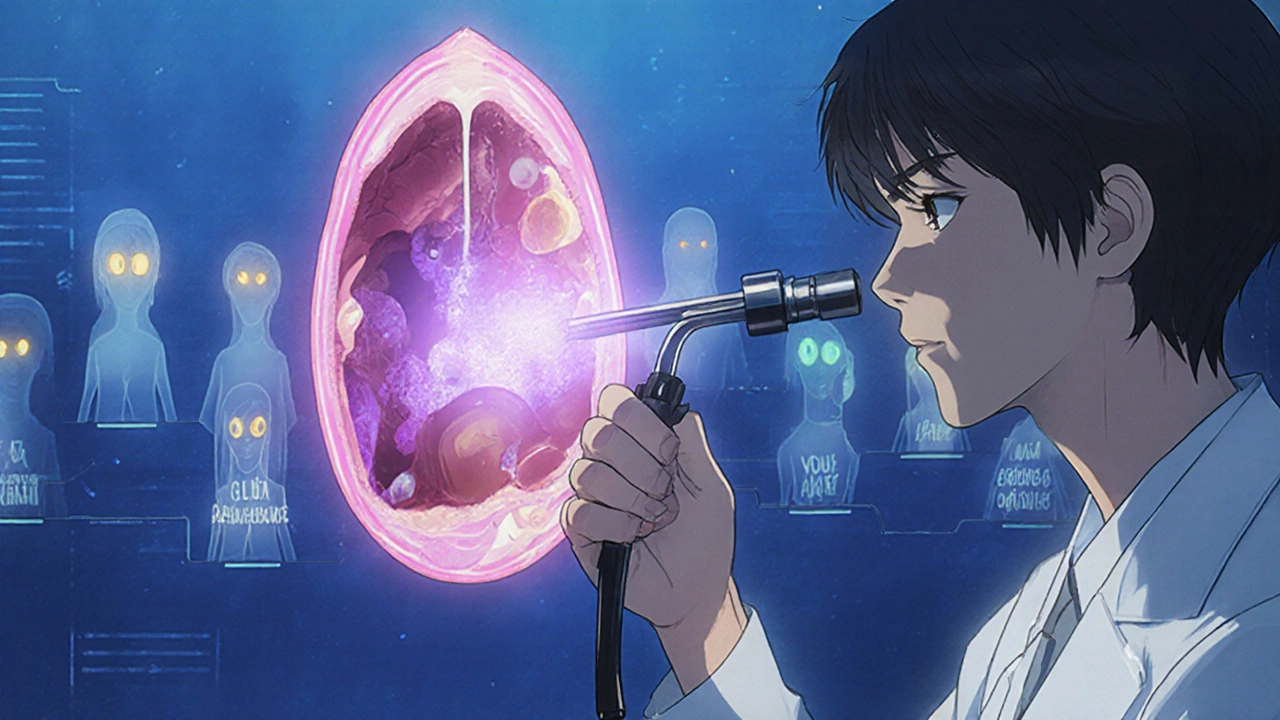
If nasal sprays and rinses aren’t enough, and you’re still having four or more sinus infections a year, it’s time to consider stronger tools. Allergy shots (immunotherapy) are one of the most effective long-term solutions. They work by slowly exposing your body to small amounts of your allergens-like ragweed or dust mites-so your immune system learns not to overreact. After 3 to 5 years of regular shots, 60-70% of patients see a big drop in sinusitis flare-ups. That’s way better than just taking pills, which only help 25-30% of the time. For those with nasal polyps and severe symptoms, biologics like dupilumab (Dupixent) have changed the game. This injectable drug targets specific parts of the immune system driving inflammation. In clinical trials, it reduced polyp size by 73% and improved breathing and sense of smell in most patients. But it’s expensive-around $3,500 a month without insurance. It’s usually only covered if you’ve tried other treatments and still struggle. Newer biologics like tezepelumab (Tezspire), approved in 2023, are showing promise too, cutting sinus flare-ups by over half in trials. These aren’t cures, but they can turn a life of constant congestion into something manageable.When to See an ENT or Allergist
You don’t need to wait until you’re in agony to get help. If you’ve tried the basics-nasal sprays, saline rinses, avoiding triggers-for 4 to 6 weeks and still feel blocked, it’s time to refer. Specific red flags include:- Nasal polyps seen on exam or imaging
- Four or more sinus infections in a year
- Symptoms lasting longer than 12 weeks
- Loss of smell or vision changes
- Severe pain, swelling around the eyes, or high fever
- History of asthma or aspirin sensitivity (which can signal AERD-Aspirin-Exacerbated Respiratory Disease)
What Most People Miss
A lot of patients focus only on the sinuses and forget the allergy part. But controlling your environment makes a huge difference. Simple steps-using HEPA filters, washing bedding weekly in hot water, keeping pets out of the bedroom, and sealing windows during high pollen season-can reduce flare-ups by 40-60%. One study found that people who avoided allergens needed 50% fewer medications. Also, don’t ignore mold. If you live in a humid climate like Melbourne, damp bathrooms, basements, or leaky roofs can harbor mold spores that trigger sinus inflammation. Antifungal nasal sprays are now being recommended for people in mold-prone areas, especially if they’ve tried everything else.The Big Picture: Breaking the Cycle
Sinusitis in allergy sufferers isn’t a one-off problem. It’s a cycle: allergies cause swelling → swelling traps mucus → mucus breeds infection → infection causes more swelling → and the cycle repeats. The only way to break it is to treat both sides: reduce the allergic trigger and calm the inflammation. That means combining environmental control, daily nasal care, and-if needed-long-term allergy treatment. Antibiotics have their place, but they’re not the answer. Biologics are powerful, but they’re not for everyone. The real win is prevention: knowing your triggers, using the right tools consistently, and seeing a specialist before things get severe. Most people with this condition spend years trying quick fixes. The truth? It takes patience. But with the right plan, you can go from feeling constantly stuffed to breathing easily-without relying on pills or antibiotics every few weeks.Can allergies cause chronic sinusitis even without infection?
Yes. Allergies trigger inflammation and swelling in the nasal passages, which blocks sinus drainage. Even without bacteria, this leads to pressure, mucus buildup, and symptoms that feel like a sinus infection. This is called allergic sinusitis, and it’s a major cause of chronic symptoms.
How long do nasal corticosteroids take to work for sinusitis?
They usually take 2 to 4 weeks of daily use to show full effect. Many people stop too early because they don’t feel immediate relief. But consistent use reduces inflammation by up to 65%, making them the most effective first-line treatment.
Are antibiotics effective for allergy-related sinusitis?
Only in about 35-45% of cases. Most allergy-driven sinusitis isn’t caused by bacteria. Antibiotics might help if symptoms last over 10 days or worsen after improvement, but they won’t stop the cycle unless the allergy is also treated.
What’s the difference between allergy shots and biologics?
Allergy shots (immunotherapy) train your immune system over 3-5 years to stop reacting to allergens like pollen or dust mites. Biologics like dupilumab target specific immune proteins causing inflammation right away, but they’re given as injections and are much more expensive. Shots are for long-term prevention; biologics are for severe, ongoing symptoms.
When should I see an ENT specialist for sinusitis?
See an ENT if you’ve tried nasal sprays and rinses for 4-6 weeks with no improvement, have four or more infections a year, have nasal polyps, or experience symptoms like loss of smell, vision changes, or severe facial pain. They can check for structural issues and recommend advanced treatments.
Can saline irrigation be dangerous?
Only if you use tap water. Untreated water can contain harmful microbes like Naegleria fowleri, which has caused rare but deadly brain infections. Always use distilled, sterile, or previously boiled (and cooled) water with your rinse device.
Do I need a CT scan for chronic sinusitis?
Not always. An ENT can often diagnose based on symptoms and nasal endoscopy. A CT scan is usually only needed if surgery is being considered or if symptoms don’t respond to treatment, to check for polyps, structural problems, or fungal infection.
Is surgery a permanent fix for sinusitis with allergies?
No. Surgery can open blocked sinuses and remove polyps, with an 85% success rate for symptom relief. But in allergy sufferers, polyps and inflammation often return within 5 years if the underlying allergies aren’t managed. Surgery helps-but it’s not a cure without ongoing allergy treatment.






Oh wow, another ‘just use saline and sprays’ guru who thinks allergies are just a lifestyle choice. Let me guess-you also think asthma is caused by not breathing ‘correctly’? I’ve had chronic sinusitis since I was 12, and no, your ‘non-drug approaches’ don’t work when your sinuses are swollen shut like a damn balloon. I’ve done the neti pot, the Flonase, the ‘avoid triggers’ nonsense. I’ve been on antibiotics so often my gut flora threw a union strike. And guess what? The only thing that actually saved me was Dupixent. Stop pretending this is about willpower. It’s biology. And if you’re not willing to go all-in on biologics, you’re just wasting everyone’s time.
Also, ‘HEPA filters help’? Cool. I live in a moldy apartment complex where the landlord thinks ‘air conditioning’ is a suggestion. Your advice is for people who live in Pinterest houses with organic hemp curtains. I’m still breathing through a straw.
And stop glorifying ‘patience.’ I’ve been patient for 18 years. My sinuses are not a Zen garden.