Many people take medications to manage chronic conditions - depression, high blood pressure, diabetes, prostate issues - but few realize how deeply these drugs can affect their sex life. Sexual side effects aren’t rare or unusual. They’re common, often overlooked, and sometimes ignored by both patients and doctors. If you’ve noticed a drop in desire, trouble getting or keeping an erection, delayed orgasm, or even numbness during sex, it might not be in your head. It could be your medicine.
Antidepressants Are the Biggest Culprit
When it comes to sexual side effects, antidepressants top the list. About 40% of people taking these medications experience some form of sexual dysfunction, according to long-term clinical studies. That number jumps even higher with certain drugs. For example, paroxetine (Paxil) causes sexual problems in up to 65% of users. Fluvoxamine (Luvox) and sertraline (Zoloft) aren’t far behind, with rates of 59% and 56% respectively. Even fluoxetine (Prozac), often thought of as milder, still affects more than half of users.
Why does this happen? Most antidepressants - especially SSRIs - increase serotonin levels in the brain. While that helps with mood, it also dampens sexual response. Serotonin acts like a brake on arousal, orgasm, and desire. The result? Many people report losing interest in sex, taking longer to reach orgasm, or not being able to climax at all.
Not all antidepressants are equal. Bupropion (Wellbutrin) and mirtazapine (Remeron) are known for having much lower rates of sexual side effects. In fact, some people even report improved libido on these drugs. If you’re struggling with sexual function on an SSRI, talk to your doctor about switching. It’s not a sign of weakness - it’s a smart adjustment.
High Blood Pressure Medications Can Kill Desire
High blood pressure is serious. But the drugs used to treat it can make sex harder - sometimes worse than the condition itself. Thiazide diuretics like hydrochlorothiazide (Microzide) are the most common cause of erectile dysfunction among heart medications. Beta blockers like atenolol and metoprolol also reduce blood flow and lower testosterone, leading to reduced arousal and performance issues.
Women aren’t spared either. About 41% of women on antihypertensives report lower sexual desire, and 34% say they feel less pleasure during sex. Alpha-blockers like clonidine and prazosin are especially linked to decreased libido.
Here’s the surprising twist: not all blood pressure drugs hurt your sex life. Angiotensin II receptor blockers like valsartan have actually been shown to improve sexual desire and fantasies in women compared to beta blockers. If you’re on a medication that’s making sex difficult, ask if switching to a different class could help. Your heart doesn’t have to suffer for your sex life to improve.
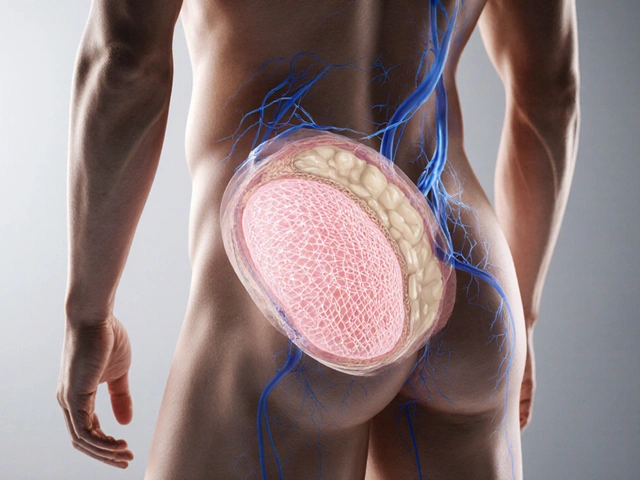
Prostate Medications and Hormone Changes
Men taking drugs for enlarged prostates or prostate cancer often face sexual side effects they weren’t warned about. 5-alpha reductase inhibitors like finasteride (Propecia) and dutasteride (Avodart) reduce dihydrotestosterone (DHT), which helps shrink the prostate - but also lowers libido, causes erectile dysfunction, and can lead to ejaculation problems. Studies show 5.9% to 15.8% of men experience reduced desire, 5.1% to 9.0% have trouble with erections, and up to 21.4% report abnormal ejaculation.
For men with prostate cancer, antiandrogens like bicalutamide are used to block testosterone. Almost all patients on these drugs lose libido, develop erectile dysfunction, and may even experience breast growth (gynecomastia). These effects are expected, but that doesn’t make them easier to handle. Pre-treatment counseling is crucial - knowing what’s coming helps men adjust emotionally and practically.

Other Surprising Offenders
It’s not just antidepressants and heart drugs. Some medications you wouldn’t suspect can also interfere with sex.
- Gabapentin and pregabalin (used for nerve pain and seizures): These can lower free testosterone by increasing sex hormone binding globulin, leading to erectile dysfunction and low desire.
- Opioids like oxycodone: They disrupt the hypothalamic-pituitary-gonadal axis, causing secondary hypogonadism - meaning your body stops making enough testosterone. This can lead to low libido and erectile problems within weeks.
- Proton pump inhibitors (PPIs) like omeprazole: Some users report decreased libido and erectile issues, though the exact mechanism isn’t clear. It may involve changes in hormone levels or nutrient absorption.
- Clomipramine (a tricyclic antidepressant): One study found 93% of users - men and women - experienced total or partial inability to orgasm.
These aren’t rare anecdotes. They’re documented patterns. If you’re on any of these drugs and notice changes in your sexual health, don’t assume it’s just aging or stress.
What Can You Do About It?
Stopping medication isn’t the answer - especially without medical guidance. But there are smart, safe ways to manage these side effects.
- Talk to your doctor. Never stop or change your dose on your own. Withdrawal from antidepressants or blood pressure meds can be dangerous.
- Switch medications. If you’re on paroxetine, switching to bupropion or mirtazapine may restore your libido. If you’re on a thiazide diuretic, asking about valsartan or another ARB could improve sexual function.
- Try a "drug holiday". For some SSRIs, taking a short break (under supervision) before planned sexual activity can help. This isn’t for everyone, but it works for some.
- Use ED medications. Studies show sildenafil (Viagra) is effective in 74% to 95% of cases for treating SSRI-induced erectile dysfunction. Tadalafil (Cialis) is another option.
- Adjust timing. Taking your antidepressant after sex instead of before can reduce interference with arousal and orgasm.
- Exercise regularly. Physical activity improves blood flow, boosts testosterone, and reduces stress - all of which help counteract sexual side effects.
For women, vaginal lubricants, pelvic floor therapy, and open communication with partners can make a big difference. For men, addressing low testosterone through testing (not just assuming it’s the drug) can reveal treatable issues.

Why This Is More Than Just an Inconvenience
Sexual side effects don’t just affect pleasure - they affect relationships, self-esteem, and mental health. Many people stop taking their antidepressants or blood pressure meds because of these effects. That’s dangerous. Depression and hypertension are serious conditions. The goal isn’t to avoid treatment - it’s to find a treatment that works for your whole life, not just your body, but your intimacy too.
Doctors are getting better at asking about this. The American Urological Association now recommends routine screening for medication-induced sexual dysfunction, especially in patients on long-term antidepressants, antihypertensives, or prostate drugs. If your doctor hasn’t asked, bring it up. You’re not being awkward - you’re being smart.
What’s Changing Now
Pharmaceutical companies are starting to take this seriously. The FDA now requires sexual side effect data in clinical trials for many CNS drugs. Researchers are testing new antidepressants that don’t spike serotonin as much. Some are even looking at genetic factors that make certain people more vulnerable to these effects - a step toward personalized medicine.
Meanwhile, studies continue to show that switching from one drug to another can dramatically improve quality of life. One woman on fluoxetine for depression switched to bupropion and reported her sex life returning to normal within six weeks. A man on hydrochlorothiazide for hypertension switched to valsartan and regained both his erections and his confidence.
There’s hope. You don’t have to live with a sex life that feels broken.
Can medication side effects cause permanent sexual dysfunction?
In most cases, sexual side effects from medications are reversible once the drug is stopped or changed. However, a small number of men report persistent erectile dysfunction or low libido after stopping finasteride or other 5-alpha reductase inhibitors - a condition sometimes called Post-Finasteride Syndrome. While rare and still being studied, it’s important to discuss long-term risks with your doctor before starting these drugs. For antidepressants and blood pressure medications, symptoms usually improve within weeks of switching or reducing the dose.
Do all SSRIs cause the same level of sexual side effects?
No. There’s a clear difference between SSRIs. Paroxetine has the highest risk, affecting up to 65% of users. Fluvoxamine and sertraline follow closely at 59% and 56%. Fluoxetine is slightly lower at 54%, while escitalopram and citalopram tend to have milder effects, around 40-45%. If sexual health is a priority, choosing escitalopram over paroxetine can make a big difference.
Can women experience sexual side effects from medications too?
Absolutely. Women report reduced libido, difficulty with arousal, delayed or absent orgasm, and decreased sexual pleasure. Antidepressants, blood pressure meds, and even hormonal birth control can contribute. Studies show 41% of women on antihypertensives report lower desire, and 34% feel less pleasure. These effects are real, common, and often underreported because people assume it’s "just how it is" - but it doesn’t have to be.
Is it safe to take Viagra with antidepressants?
Yes, in most cases. Sildenafil (Viagra) and tadalafil (Cialis) are commonly used to treat SSRI-induced erectile dysfunction. Studies show they’re effective in 74% to 95% of cases. However, always check with your doctor first - especially if you’re on nitrates for heart conditions, as combining them with ED meds can cause dangerous drops in blood pressure.
What should I do if my doctor dismisses my concerns?
Bring research. Cite specific studies - like the 59.1% incidence rate from Montejo’s study of over 1,000 patients, or the 93% anorgasmia rate with clomipramine. Ask for a referral to a specialist - a urologist, endocrinologist, or psychiatrist with experience in sexual medicine. You’re not overreacting. Medication-induced sexual dysfunction is a recognized medical issue. If your doctor won’t take it seriously, find one who will.
If you’re dealing with sexual side effects from medication, you’re not alone. And you don’t have to accept it as part of the cost of being healthy. With the right information and support, you can find a treatment plan that protects both your physical health and your intimate life.