For years, people with type 2 diabetes were told it was a lifelong, progressive condition. You’d take medication, monitor your blood sugar, and eventually add more drugs as things got worse. But that story is changing. Today, remission isn’t just a hopeful idea - it’s a real, measurable outcome for many people, and it’s mostly tied to one thing: weight loss.
What Does Remission Actually Mean?
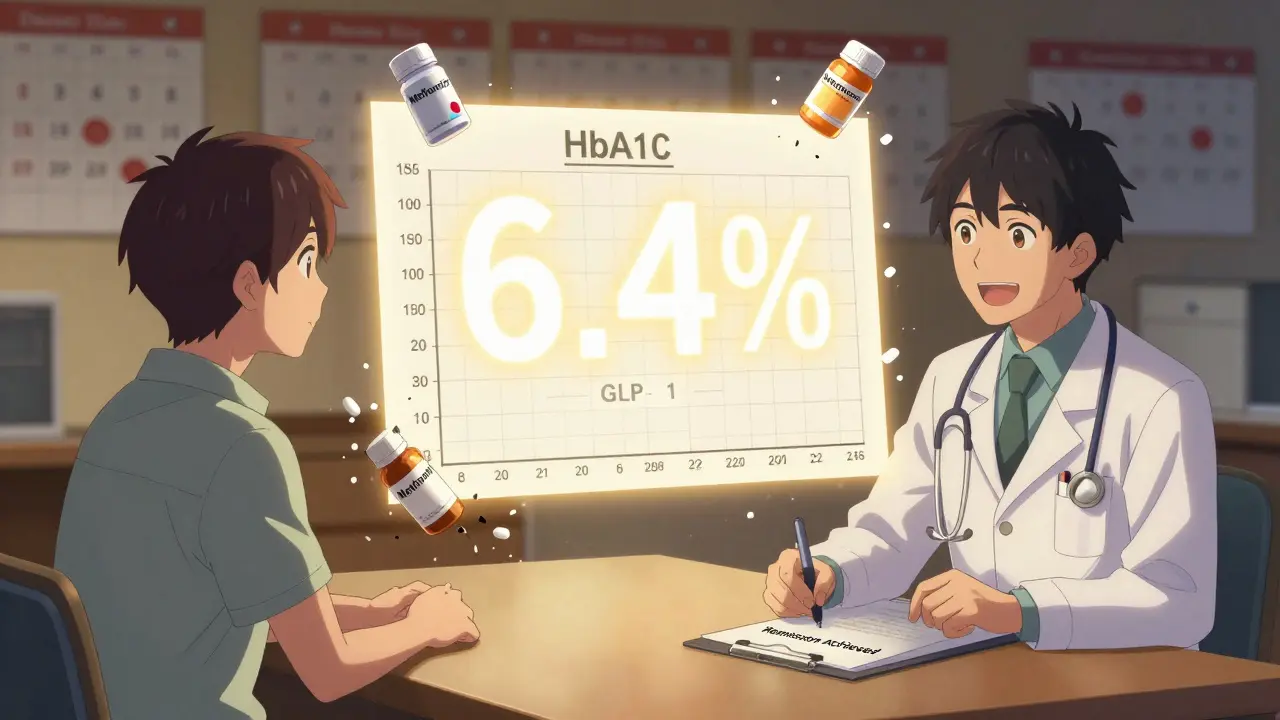
Remission in type 2 diabetes isn’t a cure. It doesn’t mean your body suddenly forgets how to have high blood sugar. It means your blood sugar levels have dropped and stayed low - without any diabetes medications - for at least three months. The official standard? Your HbA1c must be below 6.5% (48 mmol/mol). That’s the same number doctors use to diagnose diabetes. But now, if you hit it without pills, you’re in remission.
This definition wasn’t always clear. Before 2021, every study used different numbers. Some called it remission if HbA1c was below 7%, others if it lasted six months. The American Diabetes Association, Diabetes UK, the European Association for the Study of Diabetes, and the Endocrine Society came together to set one clear rule. Why? So doctors and patients could actually talk about it. If you’re not taking meds and your HbA1c is steady below 6.5%, you’re not just managing diabetes - you’re in remission.
But here’s the catch: if you’re still on metformin, GLP-1s, or insulin, and your HbA1c is low? That’s not remission. Not by this definition. The goal is to get off the meds. Not just hide the numbers.
How Much Weight Do You Need to Lose?
The data is clear: the more weight you lose, the better your chances. In the DiRECT study - a major trial run in the UK - people who lost at least 10 kilograms (about 22 pounds) had a 46% chance of remission after one year. That’s almost half. And it wasn’t surgery. It was diet. Specifically, a total diet replacement plan: low-calorie shakes for 8 to 12 weeks, then a gradual return to normal food with strong support.
But here’s what most people don’t realize: it’s not about being thin. It’s about losing fat from your liver and pancreas. When those organs get overloaded with fat, they stop working right. The pancreas can’t make enough insulin. The liver starts spilling out glucose like it’s on fire. Losing weight clears that fat. And suddenly, your body can manage blood sugar again.
Studies show that people who lost 15kg or more had over 80% remission rates. That’s huge. But even losing 5 to 10kg can make a big difference - especially if you’ve had diabetes for less than five years.
Who Has the Best Chance?
Not everyone has the same odds. Remission is more likely if:
- You’ve had type 2 diabetes for less than five years
- Your HbA1c was below 8% when you started
- You’re not on insulin
- You’re under 60 years old
- You’ve got more than 10kg to lose
People who’ve been on insulin for years? Harder. Insulin use usually means your pancreas has been struggling for a long time. That doesn’t mean it’s impossible - but it’s less likely. The same goes for people who’ve had diabetes for over ten years. Fat has been sitting on your organs too long. The damage might be too deep.
Age matters too. Younger bodies bounce back faster. But even people in their 60s and 70s have gone into remission - as long as they stick to the plan.
What Happens When You Stop Medication?
De-escalation isn’t just about stopping pills. It’s a process. You can’t just quit metformin one day and hope for the best. Your doctor will monitor your HbA1c closely - usually every 3 months - while you’re losing weight. As your blood sugar improves, they’ll slowly reduce doses. Maybe you go from two pills to one. Then to none. Only after your HbA1c stays under 6.5% for three months without any meds do you officially hit remission.
Some people worry: “If I stop my meds, will my sugar go crazy?” The answer? Not if you’re losing weight at the same time. The weight loss is what’s fixing your body. The meds were just covering up the problem. Once the root cause is addressed, the cover isn’t needed anymore.
But don’t assume you’re safe just because you’re off pills. That’s where most people slip up. You still need to eat well, move regularly, and get your HbA1c checked at least once a year. The risk of relapse is real - especially if you gain back the weight.
Remission Isn’t Forever - But It’s Still Worth It
Two years after the DiRECT study, remission rates dropped to 36%. That’s still better than the starting point. But it shows how hard it is to keep weight off. Life gets busy. Stress creeps in. Old habits return. That’s why remission isn’t a finish line - it’s a new starting point.
Still, even a few years in remission makes a difference. People who stay in remission have lower risks of heart disease, kidney damage, nerve problems, and vision loss. The longer you stay in remission, the more you delay or even prevent complications. That’s huge. You’re not just avoiding pills - you’re buying yourself more healthy years.
And here’s something most doctors don’t say out loud: being in remission changes how you see yourself. You stop feeling like a patient. You start feeling like someone who took control. That mental shift matters. It makes you more likely to keep eating well, to keep moving, to keep showing up for yourself.
What About Bariatric Surgery?
Surgery works. In the ARMMS-T2D trial, 37.5% of people who had metabolic surgery were in remission after three years. That’s impressive. But surgery isn’t for everyone. It’s expensive. It’s risky. It requires lifelong follow-up and vitamin supplements. And even then, some people still relapse.
For most people, diet and lifestyle changes are the first step. Surgery is an option if those don’t work - not the other way around. The goal isn’t to push people toward surgery. It’s to show that food, movement, and support can do something most people thought was impossible.

What’s Still Unknown?
There are big gaps. We don’t know why some people relapse and others don’t. We don’t know how long remission lasts beyond five or ten years. We don’t have enough data on whether being in remission cuts death risk. And we still don’t know the best way to help people keep the weight off long-term.
Some experts think the three-month mark is too short. Maybe it should be six months. Maybe the HbA1c cutoff should be lower - like 6.0%. Others think we need a second category: remission while on meds. If you’re on a low dose of metformin and your HbA1c is 5.8%, is that still remission? The consensus says no - but some doctors argue it should be.
For now, the rules are clear: no meds, HbA1c under 6.5%, three months steady. That’s the bar.
What Should You Do Now?
If you have type 2 diabetes and aren’t on insulin:
- Ask your doctor if you’re a candidate for remission. Don’t assume you’re too far gone.
- Get your HbA1c tested. If it’s below 8%, you have a real shot.
- Start with weight loss - not just any weight loss. Aim for at least 10kg.
- Work with a dietitian or lifestyle coach. This isn’t a DIY project. Support makes the difference.
- Track your progress. Don’t wait until you’ve lost 10kg to check your HbA1c. Test every 3 months.
- Once you’re off meds and HbA1c is steady, keep eating well. Keep moving. Keep checking in.
And if you’re already in remission? Don’t stop. You’re not cured. But you’ve done something extraordinary. Keep going. Your future self will thank you.
Can type 2 diabetes be cured completely?
No, type 2 diabetes cannot be cured. Remission means blood sugar levels are normal without medication, but the underlying tendency for high blood sugar remains. If weight is regained or lifestyle changes stop, blood sugar can rise again. Remission is a state, not a permanent fix.
Do I still need to check my blood sugar if I’m in remission?
Yes. Even in remission, you should get your HbA1c tested at least once a year. Some doctors also recommend occasional fasting glucose checks. Your risk of complications doesn’t disappear, and early signs of relapse can be caught before they become serious.
Can I stop all my diabetes meds at once?
No. Stopping medication suddenly can be dangerous. Always work with your doctor. As you lose weight, your doctor will slowly reduce your doses while monitoring your blood sugar. This prevents spikes or drops that could cause harm.
Is weight loss the only way to achieve remission?
Currently, significant weight loss is the most proven path. While some people see improvement with intense exercise or very low-carb diets alone, the strongest evidence comes from studies where weight loss of 10kg or more was the key factor. Surgery can also trigger remission, but it’s not the first-line approach.
What if I lose weight but my HbA1c doesn’t drop below 6.5%?
You may still benefit. Even if you don’t reach remission, losing weight lowers your risk of heart disease, stroke, and kidney problems. You may also need less medication. Progress isn’t all or nothing - every kilogram lost helps.
Final Thought
Remission isn’t magic. It’s science. It’s hard work. It’s not easy to lose weight and keep it off. But for many people with type 2 diabetes, it’s the only path that truly changes the game. You’re not just avoiding complications - you’re reclaiming your health. And that’s worth every step.