HIV Treatment Progress Tracker
Track Your Viral Load Progress
Enter your recent viral load readings to see your progress toward viral suppression (HIV-RNA < 50 copies/mL). This tool uses your data to estimate when you'll reach undetectable levels.
Add Your Viral Load Reading
Your Progress
Your progress toward viral suppression
Key milestone: Viral suppression (<50 copies/mL) is the goal of HIV treatment. It typically takes 8-12 weeks with Raltegravir-based regimens. Your progress will update as you add more readings.
Treatment Timeline
Click on any data point to see exact values
When you hear the name Raltegravir, you’re hearing about one of the most widely used integrase inhibitors in modern HIV care. But the drug alone isn’t the whole story. Today’s patients and clinicians rely on a suite of digital tools-from smartphone reminders to AI‑driven resistance monitoring-to make sure the medication does its job.
What is Raltegravir?
Raltegravir is a first‑generation HIV integrase strand transfer inhibitor (INSTI). It works by blocking the enzyme HIV uses to insert its genetic material into a person’s DNA, stopping the virus from replicating. Approved by the FDA in 2007, it is sold under brand names such as Isentress and is available in both 400 mg tablets and pediatric granules. Typical dosing for adults is 400 mg twice daily, while children receive weight‑adjusted amounts.
Why Integrase Inhibitors Matter
Integrase inhibitor is a class of antiretroviral drugs that target the viral integrase enzyme, a step later in the HIV life cycle than reverse‑transcriptase inhibitors. By preventing viral DNA from integrating into the host genome, these drugs achieve faster viral suppression and have a higher barrier to resistance compared with older drug classes. Raltegravir’s safety profile-few metabolic side effects and a low risk of drug‑drug interactions-makes it a go‑to option for many treatment‑naïve patients and for those switching from protease inhibitor‑based regimens.
Standard Clinical Use of Raltegravir
- First‑line therapy alongside two nucleos(t)ide reverse‑transcriptase inhibitors (NRTIs) for treatment‑naïve adults.
- Switch regimen for patients experiencing toxicity from protease inhibitors.
- Part of salvage therapy for individuals with multi‑drug resistance, especially when resistance testing shows susceptibility.
- Pregnancy category B: considered safe, but clinicians monitor liver enzymes and viral load closely.
Real‑world data from the Observational Pharmaco‑Epidemiology Research (OPERA) cohort (2023) showed that patients on a Raltegravir‑based regimen achieved viral suppression (HIV‑RNA < 50 copies/mL) in a median of 8 weeks, compared with 12 weeks for many NNRTI‑based combos.
Challenges in HIV Management
Even the best drug can stumble if patients miss doses or if resistance silently develops. Key hurdles include:
- Adherence fatigue - daily pill taking can feel burdensome.
- Stigma - fear of disclosure may lead to skipped doses.
- Access to regular monitoring - viral load and CD4 counts are essential but often delayed.
- Complex drug‑interaction landscape - especially for patients on treatment for co‑morbidities.
Technology aims to knock down these obstacles, turning a static prescription into an interactive care experience.
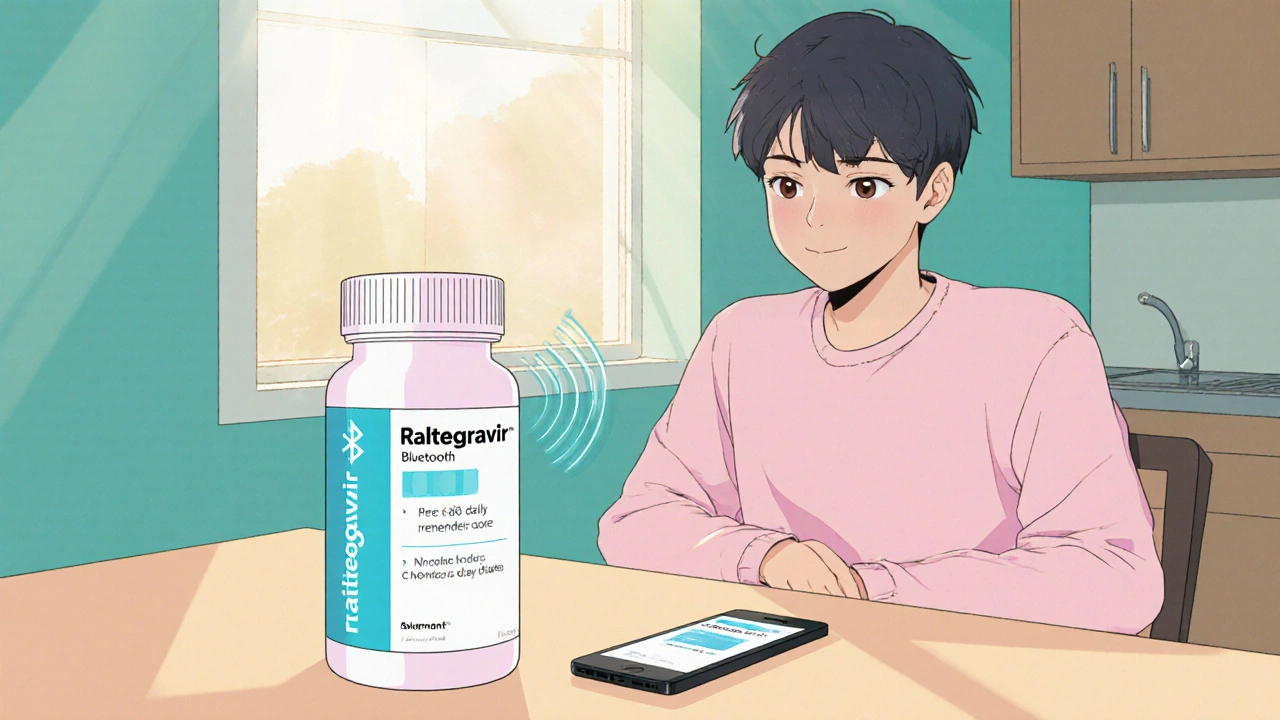
Digital Adherence Tools: The New Pillbox
Digital adherence tool refers to any electronic system-apps, smart pill bottles, or ingestible sensors-that reminds patients to take medication and records the event. A 2024 meta‑analysis of 27 randomized trials found that patients using a digital adherence solution were 23 % more likely to maintain ≥95 % adherence over six months than those relying on paper calendars.
| Tool | Primary Feature | Integration with EHR | Cost (US $ per year) | Evidence Grade |
|---|---|---|---|---|
| Smart Pill Bottle (e.g., Pill‑Track) | Bluetooth reminder + dose‑logging | Yes (HL7 FHIR) | 120 | A |
| Ingestible Sensor (e.g., Proteus) | Sensor activated by stomach fluid | Limited (custom APIs) | 350 | B |
| Mobile App (e.g., MyTherapy) | Push notifications & manual logging | Partial (via patient portal) | 0‑30 (free‑premium) | A‑ |
For a patient on Raltegravir, a smart pill bottle can send a reminder exactly when the twice‑daily dose is due, then push the data to the clinic’s electronic health record (EHR). The clinician sees a red flag if a dose is missed, allowing a timely phone call.
Telemedicine: Bridging the Clinic Gap
Telemedicine is the remote delivery of clinical services via video, phone, or messaging platforms. Since the COVID‑19 surge, the use of telehealth for HIV care surged by 68 % in the United States (CDC, 2024). It offers three big wins for Raltegravir patients:
- Convenient refill requests - patients can order the next month’s supply during a video visit.
- Rapid side‑effect assessment - a skin rash can be photographed and evaluated without a clinic trip.
- Adherence counseling - providers can review adherence dashboards in real time.
Hybrid models, where a quarterly in‑person visit is combined with monthly tele‑check‑ins, have shown higher retention rates (92 % vs 81 % in fully in‑person cohorts).
AI‑Driven Resistance Monitoring
Resistance testing used to require a lab‑draw and months of analysis. Modern AI platforms ingest viral‑load data, genotype results, and medication histories to predict emerging resistance within weeks.
One notable system, HIV‑PredictAI (2025), flags potential Raltegravir resistance when the HIV‑RNA copies climb by more than 0.5 log10 despite verified adherence. The algorithm then suggests an alternative INSTI, such as bictegravir, before resistance solidifies.
Clinicians report that AI alerts cut time‑to‑regimen‑change by an average of 14 days, translating into fewer opportunistic infections and lower healthcare costs.
Integrating Technology into Your Care Plan
Here’s a step‑by‑step guide you can hand to a patient or use in a clinic workflow:
- Choose a digital adherence tool. Ask the patient about smartphone use, comfort with Bluetooth, and budget. For most, a free app like MyTherapy paired with a low‑cost smart bottle works well.
- Set up telemedicine appointments. Schedule a video visit 30 days after initiating Raltegravir, then monthly check‑ins.
- Link data to the EHR. Work with your IT team to enable HL7 FHIR feeds from the smart bottle. Verify that missed‑dose alerts appear in the patient’s medication list.
- Enable AI resistance alerts. If your lab offers genotype sequencing, opt‑in to the AI platform. Review its dashboard before each visit.
- Monitor viral load and CD4 trends. Aim for an undetectable viral load (<50 copies/mL) within 12 weeks. Use the patient portal to let patients view their results.
By turning data into conversation, the clinician can address barriers before they become crises.
Potential Pitfalls and How to Avoid Them
Technology is powerful but not foolproof. Common issues include:
- Data overload. Clinicians may feel swamped by daily adherence logs. Set thresholds-e.g., flag only two consecutive missed doses.
- Privacy concerns. Ensure any app complies with HIPAA and local data‑protection laws. Explain to patients how their information is used.
- Device fatigue. Some patients stop using wearables after a month. Rotate reminders (push, SMS, phone call) to keep engagement fresh.
- Technical glitches. Keep a backup plan-paper diaries or a trusted caregiver can step in if the app crashes.
Future Outlook: What’s Next for Raltegravir and Tech?
By 2028, we expect three trends to reshape the landscape:
- Long‑acting injectables. Research into a Raltegravir depot that lasts 2‑3 months is in Phase II trials. If successful, adherence could become a non‑issue for many.
- Closed‑loop dosing. Smart pills that report plasma concentrations in real time could trigger automatic dose adjustments via an AI‑managed app.
- Community‑driven data pools. Anonymous, patient‑contributed data will feed machine‑learning models to predict side‑effect patterns across demographics.
Until those breakthroughs arrive, the combination of a proven drug like Raltegravir and existing digital tools provides a solid, evidence‑based roadmap for sustained viral suppression.
Key Takeaways
- Raltegravir is a safe, effective integrase inhibitor that achieves rapid viral suppression.
- Digital adherence tools, telemedicine, and AI resistance monitoring dramatically improve treatment outcomes.
- Integrating technology requires clear workflow steps, privacy safeguards, and clinician‑friendly alerts.
- Future innovations promise even easier management, but current tools already close the gap between prescription and cure.

Can I use a free app to track my Raltegravir doses?
Yes. Apps like MyTherapy or Care4Today let you set twice‑daily reminders, log each dose, and generate a printable adherence report you can share with your doctor.
Do digital tools interfere with the effectiveness of Raltegravir?
No. The tools simply remind you to take the medication and record when you do. They have no pharmacological interaction with Raltegravir.
How often should I get my viral load tested while on Raltegravir?
Guidelines recommend baseline, then at 4‑6 weeks after starting therapy, and every 3‑6 months thereafter if the viral load remains undetectable.
Is telemedicine covered by insurance for HIV follow‑up?
Most major insurers, including Medicare and Medicaid, now reimburse telehealth visits for HIV management at parity with in‑person visits.
What should I do if an AI platform flags possible resistance?
Contact your clinician promptly. They will confirm adherence data, possibly order a confirmatory genotype test, and discuss alternative regimens if needed.




Love how the article breaks down the tech tools that actually help folks stick to their Raltegravir schedule.