Beta-Blocker Psoriasis Risk Checker
This tool helps you assess your risk of psoriasis flare-ups based on the beta-blocker you're taking. Research shows some beta-blockers significantly increase psoriasis risk while others are safer options.
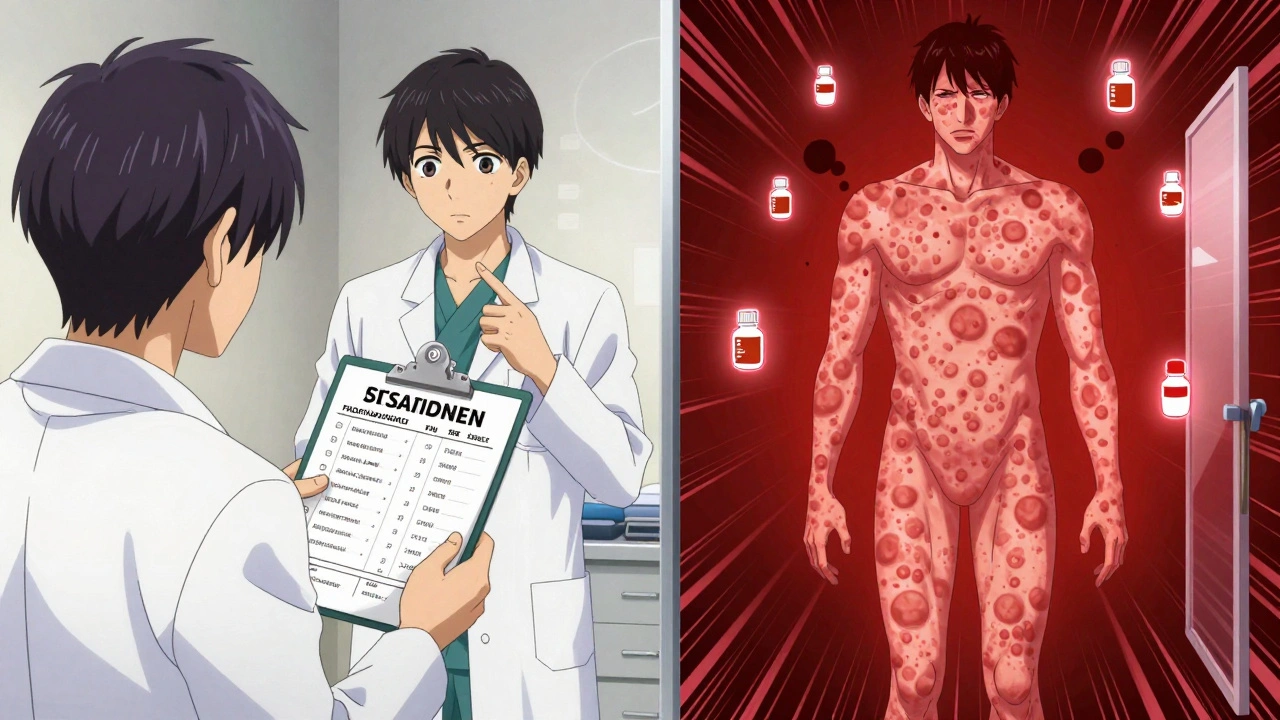
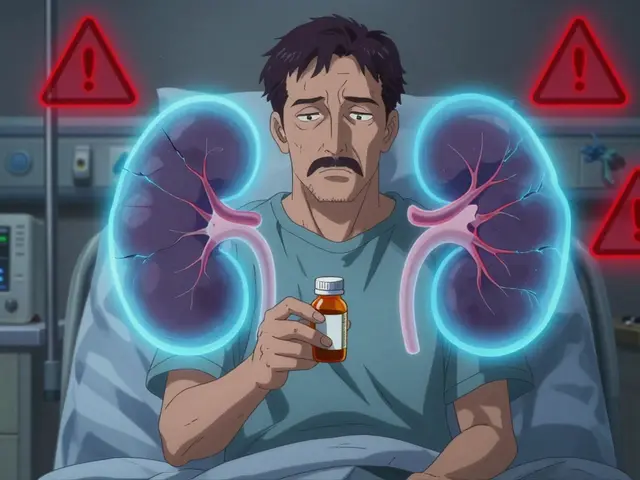
If you have psoriasis and were recently prescribed a beta-blocker for high blood pressure or heart issues, your skin flare might not be random. It could be the medication.
Why Beta-Blockers Can Trigger Psoriasis Flares
Beta-blockers like metoprolol, propranolol, and atenolol are common heart medications. They work by slowing your heart rate and lowering blood pressure by blocking adrenaline. But they don’t just affect your heart. These drugs also interfere with signaling in your skin cells.Research shows beta-blockers reduce levels of cyclic AMP (cAMP), a molecule that helps regulate skin cell growth and immune activity. When cAMP drops, skin cells multiply too fast and inflammation spikes - two hallmarks of psoriasis. This isn’t just theory. DermNet NZ reports that about 20% of people with existing psoriasis see their condition get worse after starting a beta-blocker. Some even develop psoriasis for the first time.
It’s not the same for everyone. One person might take metoprolol for months with no issues. Another sees their plaques spread within weeks. The timing is unpredictable - flares can show up anywhere from one to 18 months after starting the drug. That delay makes it easy to miss the connection.
Which Beta-Blockers Are Most Likely to Cause Problems?
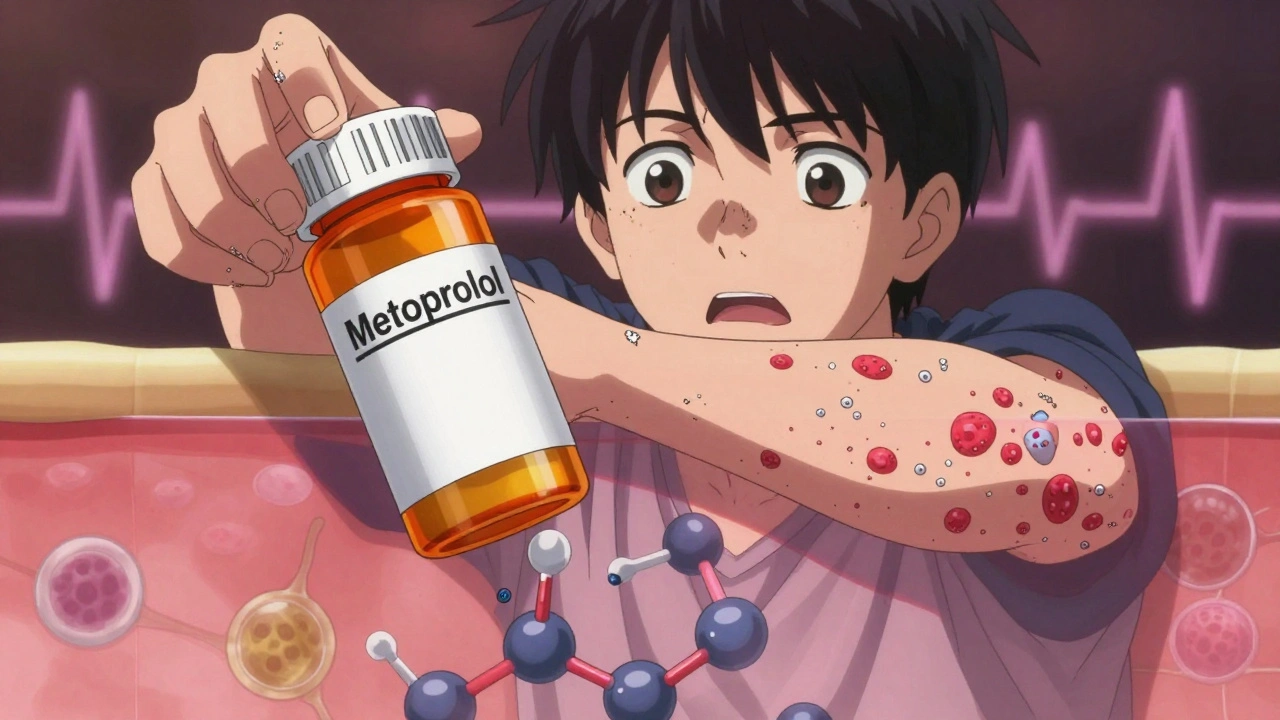
Not all beta-blockers are equal when it comes to skin reactions. Some carry a much higher risk:- Propranolol - Often linked to severe flares and even pustular psoriasis
- Metoprolol - The most commonly prescribed beta-blocker in the U.S., and one of the top triggers reported by dermatologists
- Atenolol - Associated with psoriasiform pustulosis in case reports
- Pindolol - Known to trigger pustular outbreaks
- Timolol eye drops - Used for glaucoma, but can be absorbed into the bloodstream and cause full-body psoriasis flares
Even though some beta-blockers are marketed as “cardioselective” (meaning they target the heart more than other organs), that doesn’t guarantee safety for your skin. Banner Health’s 2023 clinical guidance states that if one beta-blocker triggers a flare, others likely will too. Switching from metoprolol to atenolol won’t fix the problem - it might make it worse.
What Does the Science Say? Contradictions and Consensus
There’s conflicting research. A 2010 study in PMC2921739 argued that long-term beta-blocker use isn’t a major risk for new psoriasis. But that same study also documented multiple cases where patients developed pustular psoriasis after starting these drugs. Other studies, including a 2020 review in PMC7398737, point to clear biological pathways linking beta-blockers to skin inflammation.Here’s the real takeaway: clinical experience trumps statistical noise. Dermatologists see it every day. Patients come in with worsening plaques, and when you ask about their meds, they’re on a beta-blocker. When the drug is stopped, the skin improves - often dramatically.
The American Academy of Dermatology acknowledges beta-blockers as one of the most common drug classes linked to psoriasis flares. The European Academy of Dermatology and Venereology now recommends that doctors ask every patient with new or worsening psoriasis: “Are you on a beta-blocker?”
Real Stories: Patients Who Connected the Dots
Online communities like MyPsoriasisTeam and Reddit’s r/psoriasis are full of stories like this:“After 6 months on metoprolol, my psoriasis went from manageable to covering 30% of my body. My dermatologist asked if I was on a beta-blocker - I had no idea they could do this.” - u/PsoriasisWarrior2024, Reddit, June 2024
Another member wrote: “I thought my flare was stress-related. Turns out it was the blood pressure pill I started last year. Once I switched, my skin cleared up in weeks.”
A 2023 survey by MedicalNewsToday found that 37% of psoriasis patients on beta-blockers reported worsening symptoms - compared to just 12% of those on other blood pressure meds. The sample size was small, but the pattern matches what doctors see in clinics.
What Should You Do If You Suspect Your Medication Is Causing Flares?
Don’t stop your beta-blocker on your own. Abruptly stopping these drugs can cause dangerous spikes in blood pressure or heart rate. Instead, follow these steps:- Track your symptoms. Note when flares started, how bad they got, and whether they correlate with starting or changing your medication.
- Talk to your dermatologist. Bring your medication list. Ask specifically: “Could this be a drug-induced flare?”
- Consult your cardiologist. They need to know your skin is reacting so they can weigh risks.
- Consider alternatives. Calcium channel blockers like amlodipine or ARBs like losartan are often safer for psoriasis patients. ACE inhibitors also carry some risk, so they’re not always the best swap.
- Ask about genetic testing. Early research (like the 2024 Johns Hopkins study) suggests people with the HLA-C*06:02 gene variant may be more prone to beta-blocker-triggered flares. Testing isn’t routine yet, but it’s coming.
How Is Beta-Blocker-Induced Psoriasis Treated?
Once the trigger is removed, skin often improves on its own. But until then, standard psoriasis treatments still apply:- Topical steroids - Reduce inflammation and scaling
- Vitamin D analogues (like calcipotriene) - Slow skin cell growth
- Phototherapy - UV light treatments help calm flare-ups
- Systemic drugs (methotrexate, biologics) - Reserved for severe cases
The key is speed. The longer you stay on the triggering drug, the harder it becomes to get your skin under control. Early intervention makes a big difference.
What’s Next? New Research and Better Options
Scientists are working on next-gen beta-blockers that target only heart receptors, not skin ones. Some pharmaceutical companies are already testing compounds designed to avoid cutaneous side effects.Meanwhile, personalized medicine is gaining ground. If you have psoriasis and need a beta-blocker, knowing your genetic profile could help predict your risk. In the future, a simple cheek swab might tell your doctor whether metoprolol is safe for you - or if you should start with something else.
Bottom Line: Don’t Ignore the Link
About 8.1 million Americans have psoriasis. More than 60 million prescriptions for metoprolol alone are filled every year. That’s a huge overlap. If you’re one of the people on both lists, your skin flare isn’t just bad luck - it’s a signal.Psoriasis flares from beta-blockers are real, common, and often preventable. You don’t have to choose between heart health and skin health. With the right conversation and the right alternatives, you can manage both.
Ask your doctors. Track your symptoms. Know your options. Your skin will thank you.



So let me get this straight - we’re blaming a life-saving heart med because some people get a rash? Next they’ll say aspirin causes sneezing. Wake up. These drugs save lives. If your skin flares, tough. Stop being a snowflake.