Getting the medicine you need shouldn’t mean choosing between rent and refills. For millions of Americans, patient assistance programs from drug companies are the only way to afford life-saving drugs. But eligibility isn’t simple. It’s a maze of income limits, insurance rules, and paperwork that changes depending on who makes your medicine.
Who Qualifies for Drug Company Assistance?
The core rule across nearly all programs is income. Most require your household income to be at or below 500% of the Federal Poverty Level. For 2023, that’s $75,000 a year for one person, or $153,000 for a family of four. But that’s just the starting point.
Some programs are stricter. Pfizer’s RxPathways sets the bar at 300% FPL ($43,200 for one person) for common drugs like Eucrisa, but lifts it to 600% FPL ($77,760) for expensive cancer treatments. GSK caps income at $58,650 for a single person and $120,570 for a family of four. These aren’t arbitrary numbers-they’re tied to how much the drug costs and how much the company is willing to subsidize.
But here’s the catch: your insurance status matters just as much as your income. Most manufacturer programs require you to be uninsured or underinsured by government programs like Medicare. If you have private insurance, you’re often automatically disqualified-even if your copay is $500 a month. Merck makes an exception only for those with “special circumstances of financial and medical hardship,” which means you have to prove you’re in a crisis, not just struggling.
Medicare Patients Face a Unique Hurdle
If you’re on Medicare Part D, the rules get even more complicated. The government doesn’t want drug companies to help you pay for your meds if that help counts toward your out-of-pocket costs. So, most manufacturer PAPs are designed to work “outside” Part D. That means the free drugs you get won’t help you reach the $8,000 TrOOP threshold needed to qualify for catastrophic coverage in 2024.
Some programs, like Takeda’s Help At Hand, require you to apply for Medicare’s Extra Help program first. If you’re denied-even if you only make $19,000 a year-you can then apply for their assistance. But if you’re between 135% and 150% of the poverty line ($18,347-$20,385 for one person), you’re stuck. You don’t qualify for Extra Help, and most drug company programs won’t take you either. This gap leaves thousands without options.
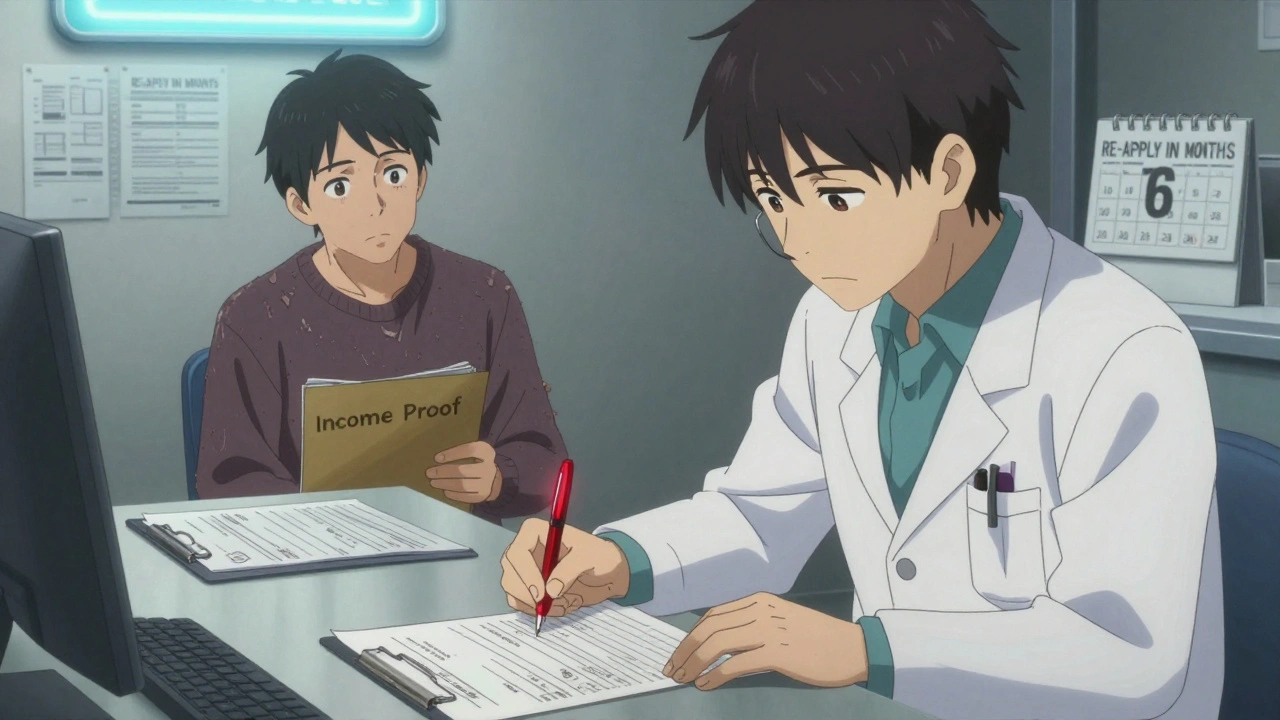
It’s Not Just About Income-Proof Matters
Applying isn’t just filling out a form. You need documents. Real ones. Pfizer wants W-2s, recent pay stubs, or your last tax return. GSK asks for proof of income from the IRS or your employer. If you’re self-employed, you might need two years of tax returns. And if you don’t have a steady job? You’ll need letters from your landlord, utility bills, or even a signed statement from a social worker.
Doctors have to sign off too. Most programs require a physician verification form-not just a prescription. That means your doctor has to confirm you’re taking the drug, that you can’t afford it, and that you’re not getting help from another source. The average wait time for a doctor’s signature? Nearly three weeks, according to Merck’s own data.
And household size? That’s where people mess up. If you live with your adult child who earns $40,000, that income counts-even if they don’t help pay for your meds. Many applicants get denied because they listed themselves as a single person when they’re actually part of a two-person household.
What Drugs Are Covered?
Not every medication is eligible. PAPs focus on high-cost drugs-especially cancer treatments, rare disease therapies, and specialty injectables. A 2023 IQVIA report found 98% of branded oncology drugs have assistance programs, compared to only 76% of heart medications.
Drug companies don’t help with generics. If your insulin costs $30 at Walmart, you won’t qualify for Abbott’s PAP for Humalog. But if your specialty insulin is $500 a month and you’re on Medicare, you might qualify.
Some programs are medicine-specific. AbbVie’s system only checks your eligibility after you pick the exact drug your doctor prescribed. You can’t apply for “help with all my meds.” You apply for Humira. Then, if approved, you get Humira. Not your blood pressure pill. Not your thyroid med. Just that one.
What Happens After You Apply?
Approval isn’t guaranteed. Reddit users on r/medicare report a 37% initial denial rate. The top reason? Incomplete paperwork. Sixty-eight percent of denials are because someone forgot to sign a form, mailed a blurry tax return, or didn’t list all household income.
Once approved, you don’t get a check. You get the medication shipped directly to your doctor’s office or pharmacy. Most people get their first supply within 72 hours. That’s faster than waiting for insurance to approve a prior authorization.
But you’re not done. Most programs require re-application every 6 to 12 months. GSK requires annual re-enrollment. Pfizer’s specialty drug programs need quarterly updates. If your income changes-even a little-you have to report it. Miss a deadline, and your meds stop.

Where to Get Help
You don’t have to figure this out alone. Seventy-eight percent of programs offer a dedicated navigator-someone who walks you through the forms. Call them. Don’t just email. Phone calls get faster responses.
Independent charities like the PAN Foundation and HealthWell Foundation are another option. They help people with private insurance who still can’t afford their copays. But they have stricter income caps-usually 400% FPL-and they cover fewer drugs.
Tools like the Medicine Assistance Tool (MAT) can help you search programs by drug name. It’s free, doesn’t collect personal info, and links directly to manufacturer portals. Use it before you start filling out forms.
What’s Changing in 2025 and Beyond?
The Inflation Reduction Act is changing the game. Starting in 2025, Medicare Part D beneficiaries will pay no more than $2,000 a year out of pocket for drugs. That’s a big deal. Experts predict 35-40% fewer Medicare patients will need PAPs after that.
But that doesn’t mean PAPs are going away. There are still 27.5 million underinsured Americans-people with insurance but sky-high deductibles and copays. Drug companies are launching new “commercial PAPs” just for them. Pfizer, Merck, and others now offer discounts to people with private insurance who pay more than $100 a month for a drug.
Still, critics argue PAPs let drugmakers avoid lowering prices. Why cut the cost of a $10,000 drug if you can just give it away for free to the people who can’t pay? The system helps individuals, but it doesn’t fix the broken pricing model.
For now, if you’re struggling to afford your meds, PAPs are your best shot. Know your income, know your insurance, gather your documents, and call the help line. Don’t wait until you run out.
Can I get free medicine if I have private insurance?
Most manufacturer patient assistance programs exclude people with private insurance. But some companies now offer separate programs for those with high out-of-pocket costs. Check if your drug maker has a “commercial PAP” or copay card. These aren’t free meds, but they can cut your monthly cost by 50-80%.
What if my income is just above the limit?
Some programs allow exceptions for medical hardship or high drug costs. If you’re making $78,000 a year but your cancer drug costs $12,000 a month, call the program. Explain your situation. They may ask for extra documentation, but they’ve approved people in similar cases before.
Do I need to reapply every year?
Yes. Most programs require annual re-enrollment. For specialty drugs, you may need to re-verify every 3-6 months. Set calendar reminders. Missing a deadline means your meds stop-no warning, no grace period.
Can I apply for multiple programs at once?
Yes. You can apply to several drug company programs if you take multiple medications. But you can’t get the same drug from two different programs. Each program covers only the drug it makes. Apply for each medication separately.
What if I’m denied?
Denials happen often-usually because of missing paperwork. Ask for the reason in writing. Fix the error. Most programs let you reapply. About 42% of people need three or more tries to get approved. Don’t give up after one denial.
Do PAPs cover over-the-counter drugs?
No. Patient assistance programs only cover prescription drugs that are branded and expensive. You won’t get free ibuprofen, insulin pens from Walmart, or asthma inhalers from CVS. These programs are for high-cost, brand-name medications only.
Are PAPs available in Australia or other countries?
No. These programs are only available to U.S. residents who are treated by U.S.-licensed doctors. If you live outside the U.S., you won’t qualify. Some countries have their own government-based assistance systems, but drug company PAPs are a U.S.-specific feature of the healthcare system.




I get that these programs help, but honestly? It’s a band-aid on a gunshot wound. Drug companies make billions and then act like saints for giving away pills they priced at $10k just to watch people beg for them. If they truly cared, they’d just lower the cost instead of making us jump through hoops like circus dogs.