Obstructive sleep apnea (OSA) isn’t just about snoring. It’s a condition where your throat muscles relax too much during sleep, blocking your airway - sometimes dozens of times an hour. Each time it happens, your brain wakes you up just enough to breathe, but not enough for real rest. Over time, this fragments your sleep, drops your oxygen levels, and puts serious strain on your heart. If you’re tired all day, wake up with headaches, or your partner says you stop breathing at night, you might have OSA. And while CPAP therapy has been the go-to solution for over 40 years, it’s not the only option - or even the best one for everyone.
What CPAP Therapy Actually Does
CPAP stands for Continuous Positive Airway Pressure. Think of it like a gentle air pump that keeps your throat open while you sleep. It’s not a cure - it’s a tool. The machine sends a steady stream of air through a mask, preventing your airway from collapsing. This isn’t new tech. It was invented in Sydney in 1981 by Dr. Colin Sullivan, and since then, it’s helped millions. Today, it’s still the gold standard for moderate to severe OSA, especially when your apnea-hypopnea index (AHI) is 15 or higher. Even for mild cases with high blood pressure or heart disease, doctors still recommend it.
Modern CPAP devices are smarter than ever. Auto-CPAP (or APAP) adjusts pressure on the fly - lower when you’re breathing fine, higher when it detects a blockage. BiPAP gives different pressures for inhaling and exhaling, which helps people who struggle with the constant force. Most machines now weigh less than 3 pounds, make about as much noise as a whisper, and connect to apps like ResMed’s AirView or Philips DreamMapper. These apps track how long you use it, how many leaks you have, and whether your AHI dropped below 5 - the target for effective treatment.
How Well Does CPAP Work? The Numbers Don’t Lie
If you use it consistently - 7+ hours a night - CPAP can slash your AHI from 39 events per hour down to 7. That’s the difference between severe OSA and near-normal breathing. Studies show it cuts daytime sleepiness by 40%, improves blood pressure by 5-10 mmHg, and boosts quality of life scores by 30-50%. One 2020 study found that after six months of consistent use, Epworth Sleepiness Scale scores dropped from 18.4 to 8.8. That’s like going from “I nap while watching TV” to “I’m alert at my desk.”
But here’s the catch: CPAP only works if you wear it. And a lot of people don’t. Around 50% of users wear their device less than 4 hours a night. Medicare and most insurers require 4 hours on 70% of nights just to keep covering it. Only about 70% of patients meet that. Even among those who stick with it, 35% report mask discomfort, 12% feel claustrophobic, and over 60% of people who start with a nasal mask end up switching to full-face because air leaks out of their mouth.
Why People Quit CPAP - And What Helps
It’s not laziness. It’s physical discomfort. A Reddit user named u/SleeplessInSeattle tried five masks over two years before switching to nasal pillows - then suddenly got 7+ hours of sleep. Another user, u/TiredButNotSleeping, said the mask felt like a prison. These aren’t rare stories. Amazon reviews show 87% of positive feedback mentions reduced snoring and better alertness. But 68% of negative reviews cite mask pain or pressure. Noise is a problem for 29%, and 42% say traveling with the machine is a nightmare.
Getting started isn’t instant. It takes 2-4 weeks to adjust. Experts recommend wearing it for 1-2 hours during the day while watching TV, then slowly building up to full nights. Heated humidifiers help 78% of people with nasal dryness. Chin straps fix mouth leaks for 65%. If your nose is congested, a saline spray or nasal dilator can make a huge difference. And don’t skip the follow-ups - sleep clinics that offer 3-5 visits in the first 90 days see much better adherence than those that just hand you the machine and say goodbye.

Oral Appliances: The Quiet Alternative
Not everyone can tolerate CPAP. That’s where oral appliances come in. These are custom-fitted devices, like mouthguards, that shift your lower jaw slightly forward to keep your airway open. They’re not as powerful as CPAP for severe cases - but they’re way easier to live with. A 2017 review from the American Academy of Dental Sleep Medicine found people use oral appliances 77% of nights after a year. CPAP? Median use is 4-5 hours per night. Four out of six studies showed patients preferred the mouthpiece.
They’re small, quiet, and travel-friendly. No hoses. No mask. Just pop it in before bed. They work best for mild to moderate OSA, or for people with severe OSA who simply won’t use CPAP. They’re not a first-line treatment for everyone, but they’re a proven backup. And they’re often covered by dental insurance - which is a big plus if your medical insurance denies CPAP.
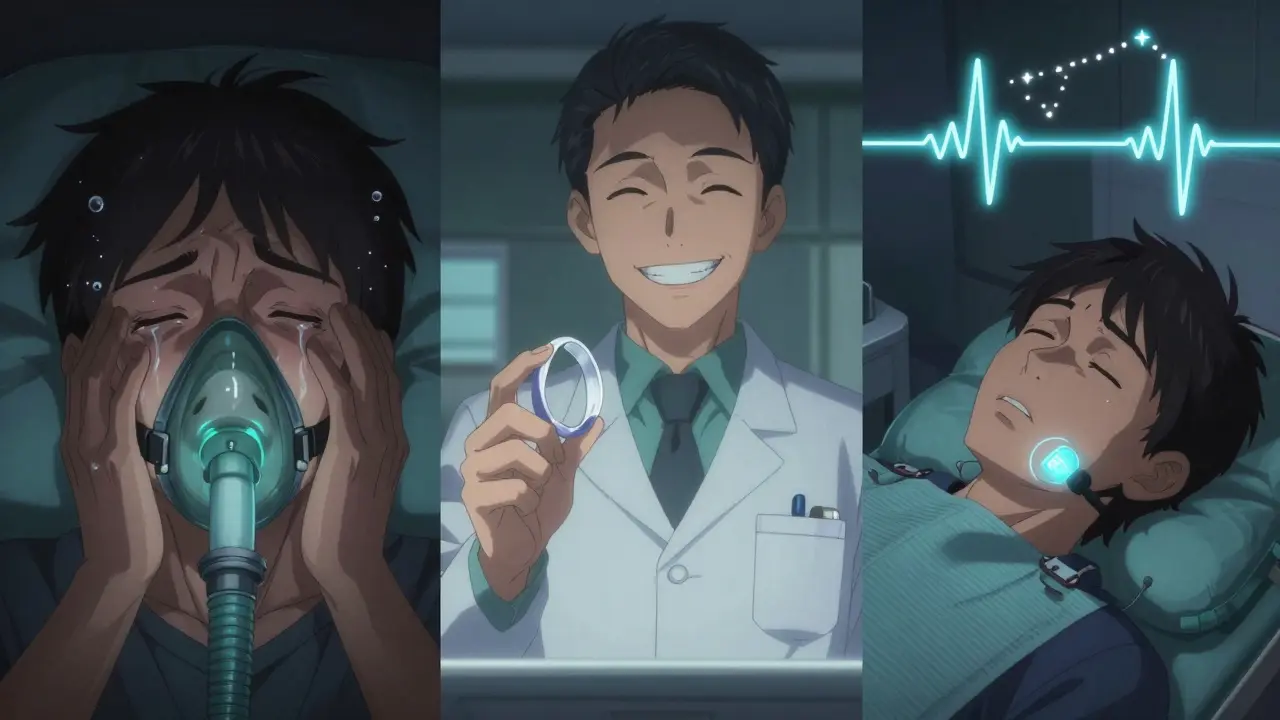
Surgery and Implants: When Other Options Fail
Surgery is rarely the first choice. Uvulopalatopharyngoplasty (UPPP) - which removes excess tissue from the throat - works for only 40-60% of people. It’s invasive, painful, and doesn’t guarantee results. Then there’s Inspire therapy: a small device implanted in your chest that stimulates the nerve controlling your tongue. It reduces AHI by 79% in clinical trials. Sounds great? It costs about $35,000 out-of-pocket and requires surgery. It’s reserved for people who can’t use CPAP or oral appliances. It’s not for everyone - but for some, it’s life-changing.
What’s Next? The Future of Sleep Apnea Treatment
Technology is evolving. ResMed’s AirSense 11, released in late 2022, detects breathing issues before they turn into full apneas. The FDA just cleared Nightware, a smartphone app that uses sound and biofeedback to train your brain to stay in deeper sleep - boosting CPAP adherence by 22% in early trials.
But the biggest shift might be personalization. Researchers now know that not all OSA patients respond the same. Dr. Andrey Zinchuk’s team found that people with high arousal thresholds - meaning they wake up easily from small breathing disturbances - get huge cognitive benefits from CPAP. It’s like a cup of coffee for their brain. But those with low thresholds? They barely notice a difference. That means CPAP might not be the right first step for everyone. The 2024 American Thoracic Society guidelines are expected to recommend testing for arousal threshold before prescribing CPAP.
Positional therapy is also gaining traction. Devices like NightBalance vibrate gently when you roll onto your back - the position that worsens OSA for many. For those with positional OSA, it reduces AHI by 51%. And there’s ongoing research into drugs that tighten upper airway muscles - no masks, no machines.
Choosing What Works for You
There’s no one-size-fits-all solution. CPAP is the most effective tool we have - if you use it. But if you can’t, oral appliances are a solid second. Surgery and implants are for rare cases. The key is matching the treatment to your life, not forcing yourself into a device that makes you miserable.
Start with a sleep study. Know your AHI. Ask your doctor about your arousal threshold. Try CPAP with support - don’t give up after a week. If it doesn’t stick, explore oral appliances. Talk to a dentist who specializes in sleep. And don’t assume surgery is your only other option - newer, less invasive tools are coming fast.
OSA is treatable. But treatment only works if it fits your life. The goal isn’t just to stop breathing interruptions - it’s to get real, restful sleep without turning your bedroom into a medical lab.
Is CPAP the only treatment for obstructive sleep apnea?
No, CPAP is the most effective treatment for moderate to severe OSA, but it’s not the only one. Oral appliances, positional therapy, and implanted devices like Inspire are proven alternatives. Surgery is an option for some, though success rates vary. The best choice depends on your OSA severity, anatomy, lifestyle, and how well you tolerate the device.
Why do so many people stop using CPAP?
Mask discomfort, claustrophobia, nasal dryness, and mouth leaks are the top reasons. About 35% of users report discomfort, 12% feel trapped, and over 60% of nasal mask users eventually switch to full-face masks because air escapes through their mouth. Machine noise and travel inconvenience also play a role. Many give up before finding the right mask or getting proper support.
How do oral appliances compare to CPAP?
Oral appliances are less effective than CPAP for severe OSA, but they have much higher adherence rates - people use them 77% of nights versus CPAP’s 4-5 hours per night on average. They’re quieter, more portable, and often preferred by users. For mild to moderate OSA, they’re a first-line alternative. For severe cases, they’re a backup when CPAP fails.
Can you outgrow obstructive sleep apnea?
Not really. OSA is usually chronic and tied to anatomy, weight, and muscle tone. Weight loss can significantly improve or even eliminate symptoms in some people - especially those with obesity-related OSA. But without ongoing management, symptoms typically return. Treatment isn’t about curing it - it’s about managing it daily.
Does insurance cover sleep apnea treatments?
Yes, most insurance plans cover CPAP machines and oral appliances if you have a diagnosed OSA and meet usage requirements. Medicare and private insurers typically require 4 hours of use on 70% of nights for 90 days. Oral appliances are often covered under dental benefits, while CPAP falls under medical. Surgery and implants like Inspire usually require prior authorization and proof of failed alternatives.