People with diabetes who take methotrexate often worry: is this drug safe for me? The short answer is yes-but only if you’re watching your blood sugar closely and working with your care team. Methotrexate isn’t a diabetes drug, but it’s commonly prescribed for autoimmune conditions like rheumatoid arthritis, psoriasis, and some types of cancer. And since many people with these conditions also have diabetes, understanding how the two interact matters more than ever.
How Methotrexate Works and Why It’s Used
Methotrexate is a disease-modifying antirheumatic drug, or DMARD. It doesn’t cure rheumatoid arthritis or psoriasis, but it slows down the immune system’s attack on your joints and skin. It does this by blocking folic acid, a vitamin your body needs to make new cells. That’s why it’s also used in cancer treatment-it stops fast-growing cells from multiplying.
Most people take methotrexate once a week, either as a pill or an injection. It’s been around since the 1950s and is one of the most studied drugs for autoimmune diseases. Millions of people take it safely every year. But if you have diabetes, you need to pay attention to how your body responds.
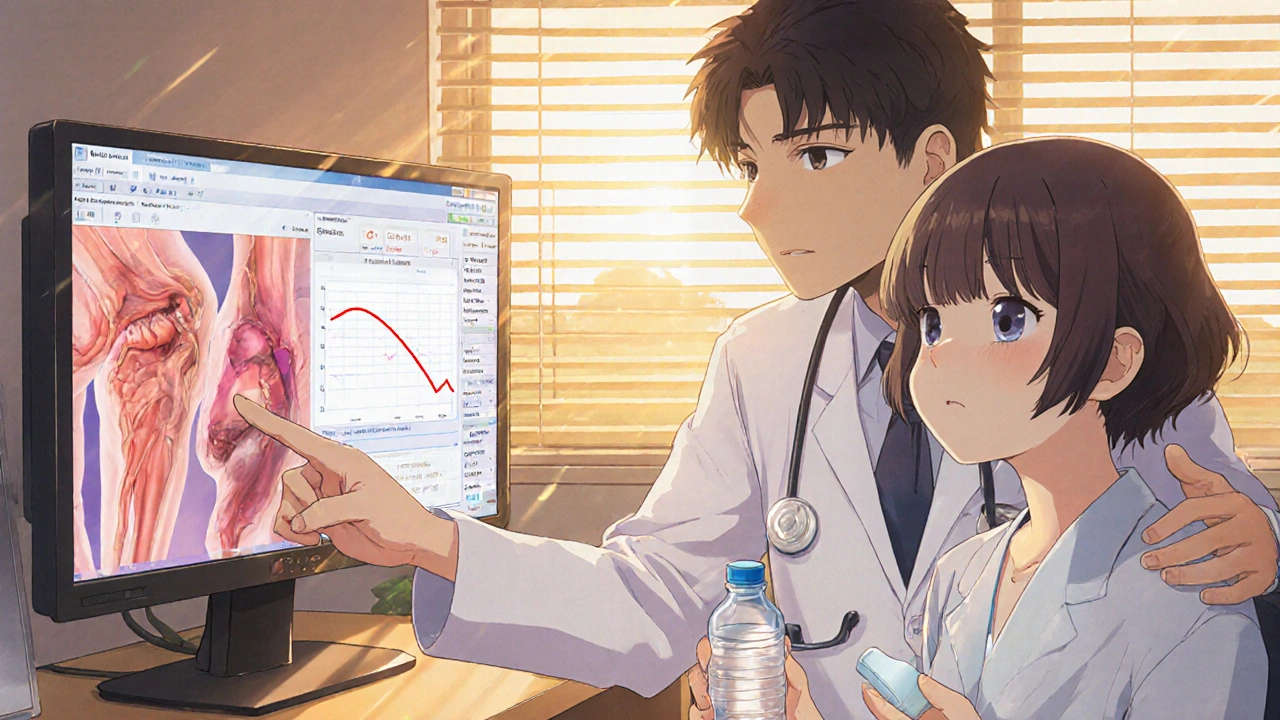
Does Methotrexate Raise Blood Sugar?
There’s no strong evidence that methotrexate directly raises blood sugar levels. Unlike steroids like prednisone-which are known to spike glucose-methotrexate doesn’t trigger insulin resistance in most people. But that doesn’t mean it’s harmless.
A 2023 study in the Journal of Clinical Rheumatology followed over 1,200 patients with rheumatoid arthritis and type 2 diabetes. Those taking methotrexate had slightly lower HbA1c levels over two years compared to those who didn’t. That’s surprising, because inflammation makes diabetes harder to control. Methotrexate reduces inflammation, which might actually help improve insulin sensitivity.
So while methotrexate doesn’t cause high blood sugar, it can change how your body handles glucose indirectly. If your inflammation drops, your insulin may start working better. That means your diabetes meds might become more effective-and you could risk low blood sugar if your doses aren’t adjusted.
What About Liver Health?
Methotrexate is processed by your liver. So is insulin and many diabetes medications. If your liver is already stressed from fatty liver disease-which is common in people with type 2 diabetes-methotrexate can add extra strain.
Doctors check liver enzymes (ALT, AST) before starting methotrexate and every few months after. If your numbers are high, they may lower your dose or stop the drug. Fatty liver disease is often silent, so even if you feel fine, you could have it. A simple ultrasound or FibroScan can tell you more.
Alcohol makes this worse. If you drink even one or two drinks a week, your risk of liver damage from methotrexate goes up. Many people with diabetes are told to limit alcohol anyway-but with methotrexate, it’s not just about calories. It’s about protecting your liver.
Kidney Function and Drug Clearance
Your kidneys help clear methotrexate from your body. If your kidney function is low-which happens more often with long-term diabetes-you could build up too much of the drug. That increases the risk of side effects like nausea, mouth sores, or even bone marrow suppression.
Doctors measure kidney function with a blood test called eGFR. If your eGFR is below 60, they’ll usually reduce your methotrexate dose. If it’s below 30, they might avoid it entirely. Some people with diabetes don’t realize their kidneys are declining until it’s advanced. Regular checkups are non-negotiable.
Drug Interactions to Watch For
Methotrexate can interact with several common diabetes medications:
- Metformin: Both are cleared by the kidneys. Taking them together might raise the risk of kidney buildup. Your doctor might space them out or lower the dose.
- NSAIDs (like ibuprofen or naproxen): These can block methotrexate from leaving your body. Many people with arthritis take NSAIDs for pain. If you’re on methotrexate, avoid them unless your doctor says it’s safe.
- Sulfonylureas (like glipizide): These can cause low blood sugar. If methotrexate improves your insulin sensitivity, your risk of hypoglycemia goes up. Watch for shakiness, sweating, or confusion.
- Diuretics (water pills): These can reduce kidney function and raise methotrexate levels. Be extra careful if you’re taking furosemide or hydrochlorothiazide.
Always tell your pharmacist and doctor about every medication, supplement, and herb you take-even over-the-counter ones. Some cold medicines contain NSAIDs. Some supplements have high doses of folate, which can interfere with methotrexate’s effect.
What You Should Do Daily
If you’re on methotrexate and have diabetes, here’s what to do every day:
- Check your blood sugar more often-especially when you start methotrexate or change your dose. You might see unexpected drops.
- Take folic acid as prescribed. Most doctors give 1 mg daily (except on your methotrexate day). This cuts down on side effects like nausea and mouth sores without reducing the drug’s effectiveness.
- Avoid alcohol completely. No exceptions.
- Stay hydrated. Drink at least 8 glasses of water a day to help your kidneys flush out the drug.
- Watch for signs of infection. Methotrexate lowers your immune response. Fever, sore throat, or a cough that won’t go away? Call your doctor.
When to Call Your Doctor
Don’t wait for your next appointment if you notice:
- Unexplained low blood sugar (below 70 mg/dL) that doesn’t match your diet or activity
- Yellowing of the skin or eyes (sign of liver problems)
- Dark urine or swelling in your legs (kidney warning signs)
- Severe fatigue, dizziness, or bruising easily (possible bone marrow issue)
- Persistent nausea, vomiting, or mouth sores
These aren’t common-but they’re serious. Early action can prevent hospitalization.
Alternatives If Methotrexate Isn’t Safe for You
If your liver or kidneys can’t handle methotrexate, or if your blood sugar gets too unstable, there are other options:
- Sulfasalazine: Another DMARD, gentler on the liver, often used for rheumatoid arthritis.
- Leflunomide: Works similarly to methotrexate but may be easier on kidneys in some people.
- Biologics: Drugs like adalimumab or etanercept target specific parts of the immune system. They don’t affect the liver the same way and are often safe with diabetes.
Your rheumatologist and endocrinologist should talk to each other. A team approach gives you the best shot at managing both conditions safely.
Bottom Line: You Can Take Methotrexate With Diabetes
Methotrexate isn’t off-limits if you have diabetes. In fact, it might help your blood sugar by reducing inflammation. But it’s not a set-it-and-forget-it drug. You need regular blood tests, careful monitoring of your glucose levels, and honest conversations with your doctors.
The biggest risk isn’t methotrexate itself-it’s assuming everything’s fine because you feel okay. Diabetes and autoimmune diseases are both silent until they’re not. Stay ahead of it. Check your numbers. Ask questions. Don’t skip your labs. Your long-term health depends on it.
Can methotrexate cause low blood sugar?
Methotrexate doesn’t directly lower blood sugar, but it can reduce inflammation, which may improve insulin sensitivity. This can make diabetes medications work better, leading to unexpected low blood sugar. If you’re on insulin or sulfonylureas, check your glucose more often when starting or adjusting methotrexate.
Is it safe to drink alcohol while taking methotrexate with diabetes?
No. Alcohol increases the risk of liver damage when combined with methotrexate. People with diabetes are already at higher risk for fatty liver disease. Drinking even small amounts can push your liver into failure. Avoid alcohol completely while on this medication.
Does methotrexate damage the kidneys in people with diabetes?
Methotrexate is cleared by the kidneys, and diabetes can reduce kidney function over time. If your eGFR drops below 60, your doctor will lower your methotrexate dose. If it’s below 30, they’ll likely stop it. Regular kidney tests are essential to avoid buildup and toxicity.
Can I take NSAIDs like ibuprofen with methotrexate and diabetes?
Avoid NSAIDs like ibuprofen or naproxen unless your doctor approves them. These drugs can block methotrexate from leaving your body, raising its levels and increasing side effects. They can also harm your kidneys, which is risky if you have diabetes.
Should I take folic acid with methotrexate if I have diabetes?
Yes. Most doctors prescribe 1 mg of folic acid daily (except on your methotrexate day). It reduces side effects like nausea and mouth sores without affecting how well methotrexate works. This is especially important if you have diabetes, since poor nutrition can make both conditions harder to manage.
What’s the best way to monitor my health while on methotrexate and diabetes?
Check your blood sugar daily, get liver and kidney tests every 3-6 months, and have your HbA1c checked every 3 months. Keep a log of any unusual symptoms-fatigue, nausea, bruising, or unexplained low blood sugar. Bring this to every appointment. Communication with both your rheumatologist and endocrinologist is key.




Methotrexate doesn't raise blood sugar? Interesting. I've been on it for 3 years, and my A1c went from 6.8 to 7.9... coincidence? Maybe. But I'm not buying the 'it helps insulin sensitivity' story. My endo says my liver enzymes are elevated too. So... maybe it's not the miracle drug they say it is? Just saying.