When treating fungal skin infections that also cause inflammation, Lotrisone is a prescription cream that pairs the corticosteroid betamethasone dipropionate with the antifungal clotrimazole. It’s aimed at conditions like athlete’s foot, jock itch, and contact dermatitis where you need both anti‑inflammatory and antifungal action.
What makes Lotrisone different?
Lotrisone’s unique selling point is the fixed‑dose combination of two active ingredients:
- Betamethasone is a potent topical corticosteroid that reduces redness, swelling, and itching.
- Clotrimazole is a broad‑spectrum azole antifungal that stops the growth of dermatophytes and yeasts.
Because the two act together, doctors often prescribe Lotrisone for mixed‑type skin issues that would otherwise need two separate products.
When should you consider an alternative?
Even though the combo works well, there are scenarios where an alternative might be a better fit:
- You have a mild fungal infection without significant inflammation - a pure antifungal can spare you unnecessary steroid exposure.
- You’re looking for an over‑the‑counter (OTC) option to avoid a prescription.
- You’ve experienced side‑effects from corticosteroids, such as skin thinning or hormonal disturbances.
- Cost is a concern; some alternatives are cheaper, especially in generic form.
Key criteria for comparing Lotrisone with other topicals
To make a fair comparison, line up the same attributes for each product:
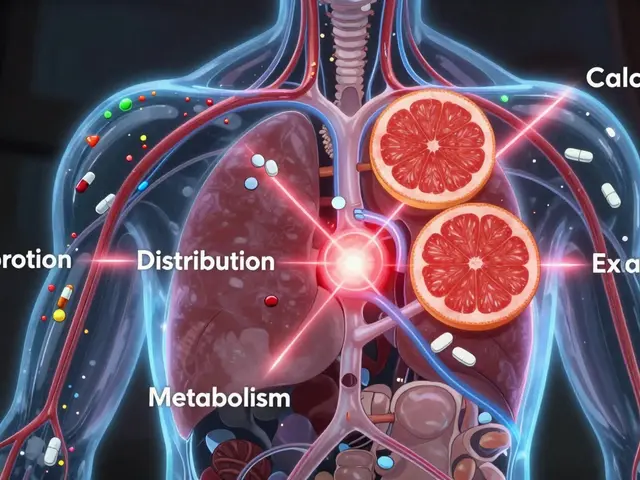
- Active ingredient(s) and their mechanism
- Prescription vs. OTC status
- Typical dosage strength and application frequency
- Common side‑effects
- Average retail cost (US, 2025)
- Conditions officially approved

Comparison table of popular alternatives
| Product | Active ingredient(s) | Prescription? | Typical use | Key side‑effects | Avg. price (30 g) |
|---|---|---|---|---|---|
| Lotrisone | Betamethasone dipropionate + Clotrimazole | Prescription | Inflamed fungal infections | Skin thinning, burning | $30 |
| Hydrocortisone 1% + Miconazole | Hydrocortisone + Miconazole nitrate | Prescription | Similar to Lotrisone, milder steroid | Minor irritation | $25 |
| Clotrimazole 1% cream | Clotrimazole | OTC | Pure fungal infections | Rare allergic reaction | $12 |
| Terbinafine 1% cream | Terbinafine | OTC | Dermatophyte infections (athlete’s foot) | Dryness, mild burning | $15 |
| Ketoconazole 2% shampoo | Ketoconazole | OTC | Scalp and body fungus | Scalp irritation | $10 |
| Lamisil AT (Terbinafine) gel | Terbinafine | Prescription | Severe tinea infections | Itching, redness | $35 |
Deep dive into each alternative
Hydrocortisone + Miconazole combo
This product pairs a low‑potency steroid (hydrocortisone) with an azole antifungal (miconazole). It’s a step‑down option for patients who need anti‑inflammatory help but want to avoid the strength of betamethasone. Hydrocortisone offers mild corticosteroid activity, suitable for delicate skin areas. Meanwhile, Miconazole covers a broad range of dermatophytes and Candida species. The combo is prescription‑only in the U.S. but generally cheaper than Lotrisone.
Clotrimazole 1% cream (OTC)
If inflammation is minimal, a straight antifungal often suffices. Clotrimazole inhibits fungal ergosterol synthesis, halting cell membrane formation. The 1% cream is widely available without a doctor’s note, making it a go‑to for athlete’s foot or jock itch. Side‑effects are rare-mostly mild skin irritation.
Terbinafine (OTC and prescription)
Terbinafine belongs to the allylamine class and attacks the fungal enzyme squalene epoxidase, leading to cell death. It works faster than many azoles, often clearing infections in under two weeks. The OTC 1% cream is popular for tinea pedis, while the prescription gel (Lamisil AT) tackles tougher cases.
Ketoconazole shampoo
This is the only antifungal on the list that’s formulated as a shampoo, useful for scalp ringworm or body‑wide fungal spread. Ketoconazole blocks ergosterol synthesis similar to other azoles but with strong activity against Malassezia. It’s an OTC option, though some dermatologists recommend a prescription‑strength version for stubborn cases.
Pros and cons at a glance
- Lotrisone: strong anti‑inflammatory plus antifungal; prescription ensures proper use; higher cost; risk of steroid‑related skin thinning.
- Hydrocortisone + Miconazole: milder steroid; still prescription; slightly cheaper; may need longer treatment.
- Clotrimazole: OTC, cheap, no steroid side‑effects; not effective for inflamed lesions.
- Terbinafine: fast‑acting, OTC for mild cases; no steroid; may irritate dry skin.
- Ketoconazole shampoo: excellent for scalp, OTC; limited to surface applications; can cause hair dryness.
How to choose the right product for you
Follow this quick decision tree:
- Is there noticeable redness, swelling, or itching? - Yes: consider a steroid‑containing option (Lotrisone or Hydrocortisone + Miconazole). No: move to step 2.
- Do you need an OTC solution? - Yes: try Clotrimazole or Terbinafine. No: discuss prescription options with your doctor.
- Is the infection on the scalp or a large body area? - Yes: Ketoconazole shampoo may be optimal.
- Are you sensitive to steroids or have a history of skin thinning? - Yes: skip steroid combos and stick with pure antifungals.
Always finish the full course, even if symptoms improve early. Stopping too soon can let the fungus rebound.
Frequently asked questions
Can I use Lotrisone for a simple athlete’s foot?
If the foot only has mild fungal growth without redness, a plain antifungal like clotrimazole or terbinafine is usually enough. The steroid in Lotrisone isn’t needed and adds a risk of skin thinning.
How long should I apply Lotrisone?
Doctors typically advise a 2‑week course, applying a thin layer twice daily. Do not exceed the prescribed time without consulting your clinician.
Are there any drug interactions with Lotrisone?
Because it’s a topical, systemic interactions are rare. However, avoid using other potent topical steroids on the same area unless directed by a physician.
Is it safe to use Lotrisone on children?
Pediatric use is allowed but usually limited to short periods and low‑dose formulations. Always follow a pediatrician’s guidance.
What does Lotrisone alternatives mean for my insurance?
Many insurers cover prescription Lotrisone but may require prior authorization. OTC alternatives like clotrimazole or terbinafine usually don’t need approval, which can lower out‑of‑pocket costs.




Look, anyone who thinks a combo cream like Lotrisone is the be‑all and end‑most of dermatology is simply ignoring the vast resources our nation pours into pharmaceutical innovation. The United States leads the world in developing cutting‑edge topical therapies, and Lotrisone is a prime example of that superiority. Yet, the average consumer is still being sold a pricey prescription without considering that cheaper, free‑standing antifungals perform just as well for mild cases. In short, we should demand smarter prescribing that reflects both efficacy and fiscal responsibility.