Liver Drug Clearance Calculator
This calculator helps estimate how liver disease affects your body's ability to clear medications. Based on your liver function score, it shows approximate clearance reduction and provides guidance on dose adjustments for common medications.
Select Your Liver Function Assessment
Estimated Clearance Reduction
Select your liver function assessment and click Calculate to see results.
Important Safety Information
These estimates are approximate. Actual dose adjustments depend on:
- Specific medication properties
- Your age and other health conditions
- Other medications you're taking
- Individual response to drugs
When your liver is damaged, it doesn’t just affect how you feel-it changes how your body handles every pill you take. Many people don’t realize that common medications like painkillers, sedatives, and even antibiotics can build up to dangerous levels in the body if you have liver disease. This isn’t theoretical. It’s happening right now in clinics across the U.S., where over 22.5 million people live with chronic liver conditions. The result? Higher risk of overdose, confusion, falls, and even coma-not because the drugs are weak, but because the liver can’t clear them like it used to.
Why the Liver Matters for Drug Clearance
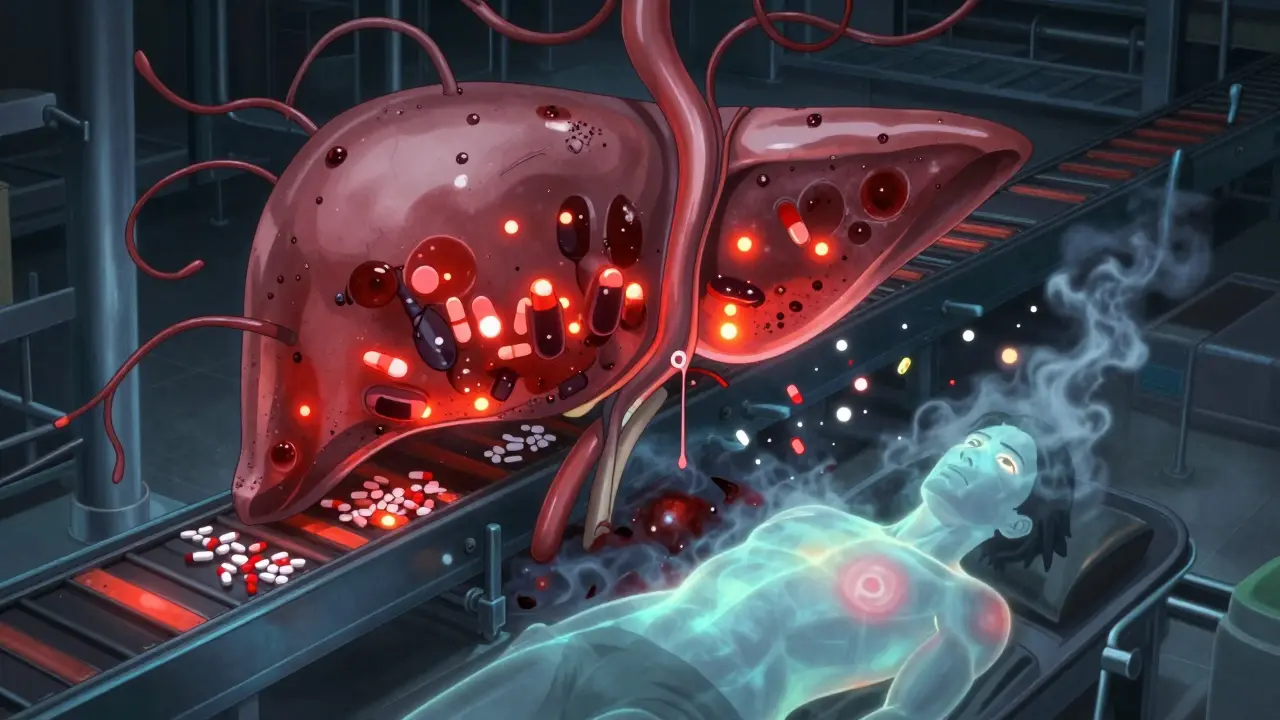
Your liver doesn’t just process alcohol or detoxify poisons. It’s the main factory for breaking down most medications. About 70% of the drugs you take-everything from antidepressants to blood thinners-are metabolized there. Two key systems do this work: the cytochrome P450 enzymes (like CYP3A4 and CYP2E1) and transport proteins (like OATP1B1). In healthy people, these work like a well-oiled assembly line. In liver disease, the line breaks down.Advanced liver disease, especially cirrhosis, causes real physical damage. Liver cells die. Scar tissue forms. Blood flow slows. And the enzymes that break down drugs? Their activity drops by 30% to 70%, depending on the drug and how bad the damage is. That means drugs stick around longer. Instead of being cleared in a few hours, they linger for days. This is called reduced clearance.
High-Extraction vs. Low-Extraction Drugs: Not All Medicines Are the Same
Not every drug behaves the same way in a damaged liver. The difference comes down to how the liver handles them.High-extraction drugs (like fentanyl, morphine, and propranolol) rely on blood flow. If the liver isn’t getting enough blood-because of scarring or shunting-these drugs aren’t cleared well. Their levels can spike fast, even with normal doses.
Low-extraction drugs (like diazepam, lorazepam, and methadone) depend on enzyme activity. Since liver enzymes are impaired in cirrhosis, these drugs build up slowly but steadily. And here’s the kicker: about 70% of commonly prescribed drugs fall into this category. That means most of the pills you’re taking are at risk.
Take benzodiazepines, for example. Diazepam has active metabolites that stick around for days. In someone with cirrhosis, those metabolites can accumulate to toxic levels, causing drowsiness, confusion, or even hepatic encephalopathy. Lorazepam, on the other hand, doesn’t form active metabolites. It’s cleared more directly-and even though clearance is still reduced, the risk is lower. That’s why doctors often switch patients from diazepam to lorazepam.
What Happens When Drugs Build Up
When drugs aren’t cleared properly, the effects aren’t just stronger-they’re more dangerous.One of the most serious risks is hepatic encephalopathy. This is when toxins build up in the brain because the liver can’t filter them out. Opioids and sedatives make this worse. In people with cirrhosis, their brains become 30% to 50% more sensitive to these drugs. A standard dose of morphine that’s safe for a healthy person can cause coma in someone with liver disease.
Warfarin, a blood thinner, is another example. Its clearance drops by 30% to 50% in cirrhosis. If you don’t adjust the dose, the INR (a measure of blood clotting) can climb dangerously high. That means a minor bump could lead to internal bleeding. Studies show that patients with cirrhosis often need 25% to 40% less warfarin to stay in the safe range.
Antibiotics like ceftriaxone are another surprise. Standard doses can cause peak concentrations 40% to 60% higher in cirrhotic patients. That’s why many hepatologists now use lower doses-even though guidelines haven’t fully caught up.
How Doctors Measure Liver Damage-And Why It Matters
You can’t just look at a single lab test to know how your liver is handling drugs. That’s why doctors use two systems: Child-Pugh and MELD.Child-Pugh scores liver function based on five things: bilirubin, albumin, INR, ascites, and mental status. Class A is mild, Class B is moderate, Class C is severe. For drugs cleared by the liver:
- Class B: Reduce dose by 25% to 50%
- Class C: Reduce dose by 50% to 75%
MELD score (based on bilirubin, INR, and creatinine) is more precise for predicting outcomes. For every 5-point increase in MELD above 10, drug clearance drops by about 15%. That’s why some hospitals now use MELD to guide dosing for critical medications.
But here’s the hard truth: even these scores aren’t perfect. Drug levels don’t always match the numbers on a lab report. Two people with the same MELD score can metabolize the same drug very differently. That’s why therapeutic drug monitoring-measuring actual drug levels in the blood-is becoming essential for drugs with narrow safety margins, like digoxin, tacrolimus, or phenytoin.
What About Newer Drugs? Are They Safer?
The pharmaceutical industry is finally catching on. In 2023, the FDA approved 18 new drugs with specific dosing instructions for liver disease-up 25% from 2022. Nearly all new drug applications now include studies on hepatic impairment, compared to just 65% in 2018.Some drugs are naturally safer. Sugammadex, used to reverse muscle relaxants during surgery, is 96% cleared by the kidneys. So even in advanced liver disease, no dose change is needed. But here’s the catch: recovery time was 40% longer in transplant patients. That’s because other organs are stressed too.
And then there’s MASLD-metabolic dysfunction-associated steatotic liver disease, formerly called fatty liver. It affects 30% of Americans. Even in early stages, before scarring, CYP3A4 activity drops by 15% to 25%. That means people with “mild” fatty liver might still need lower doses of statins, antidepressants, or pain meds. Most doctors still don’t realize this.
What Should You Do?
If you or someone you care for has liver disease, here’s what you need to do:- Know your Child-Pugh or MELD score. Ask your doctor for it.
- Ask about every medication: “Is this cleared by the liver? Do I need less?”
- Don’t assume over-the-counter drugs are safe. Acetaminophen (Tylenol) is fine in small doses-but too much can be deadly in liver disease.
- Watch for signs of drug buildup: confusion, extreme sleepiness, dizziness, nausea, or tremors.
- Ask if therapeutic drug monitoring is an option. It’s not always offered, but it can save your life.
Pharmacists are now playing a bigger role too. Between 2020 and 2023, pharmacist-led dose adjustment services for liver patients increased by 40%. Don’t be afraid to ask your pharmacist to review your full list of medications.
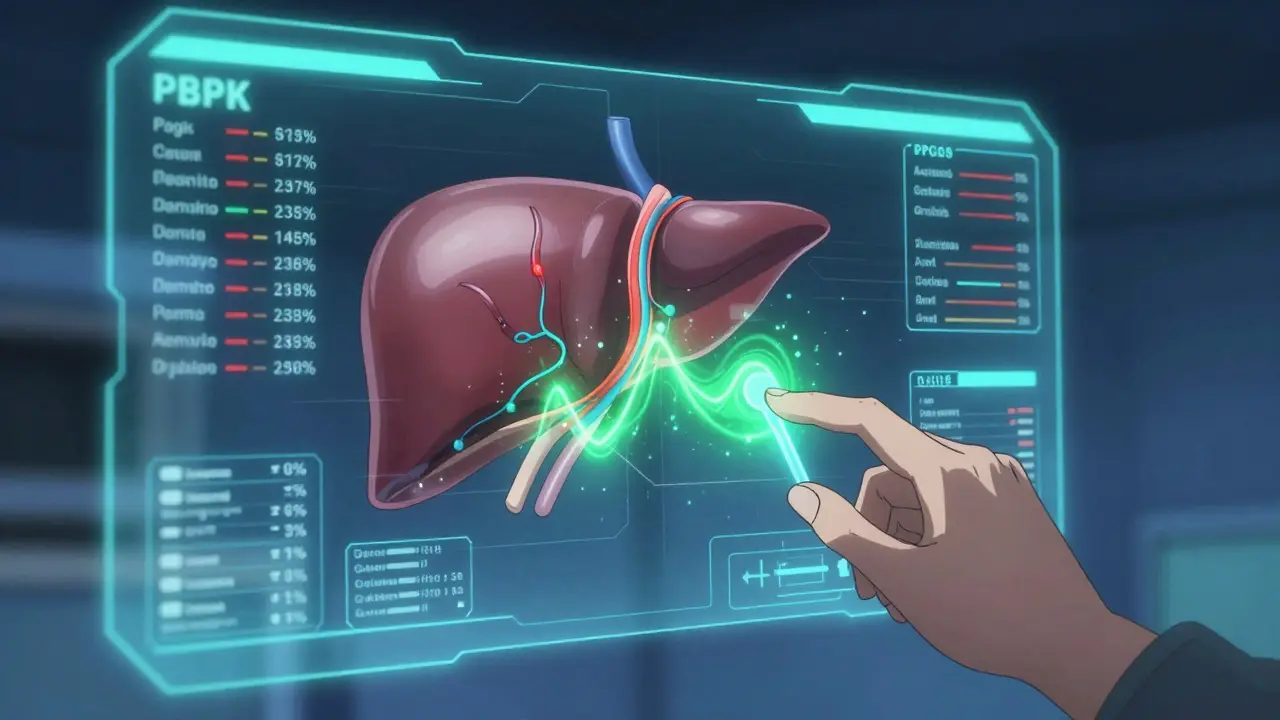
The Future: Personalized Dosing Is Coming
The old way of dosing-“one size fits all”-is fading. New tools like physiologically based pharmacokinetic (PBPK) modeling can now predict how a drug will behave in a specific patient, based on liver blood flow, enzyme levels, and shunting. These models are 85% to 90% accurate.Within five years, most new drug labels will include model-based dosing recommendations. And soon after, genetic testing will join the picture. For example, if you carry the CYP2C9*3 allele (found in 8.3% of Caucasians), you break down warfarin even slower. Combine that with cirrhosis, and you’re at extreme risk.
What’s clear is this: liver disease isn’t just about the liver. It’s about how every drug you take interacts with your body’s broken system. Ignoring it isn’t an option. Adjusting doses isn’t overcautious-it’s lifesaving.
Can I still take painkillers if I have liver disease?
Yes-but with serious limits. Acetaminophen (Tylenol) is generally safe at 2,000 mg per day or less for people with liver disease. Avoid NSAIDs like ibuprofen or naproxen-they can harm the kidneys and worsen fluid retention. Opioids like oxycodone or hydrocodone should be used only if absolutely necessary, and at much lower doses. Always check with your doctor before taking any painkiller.
Do herbal supplements affect drug metabolism in liver disease?
Absolutely. Many herbs-like milk thistle, kava, green tea extract, and black cohosh-are processed by the liver and can interfere with drug-metabolizing enzymes. Some may even cause liver injury themselves. There’s no safety data for most supplements in cirrhosis. If you’re taking them, tell your doctor. Better yet, stop them unless they’re medically approved.
Why do some drugs need no dose adjustment in liver disease?
Two reasons: either the drug is cleared mostly by the kidneys (like sugammadex or most antibiotics), or it’s metabolized by the liver but in very small amounts (less than 20%) and has a wide safety margin (like some antacids or antihistamines). These are the exceptions-not the rule. Most drugs require some adjustment.
Can liver disease get worse because of medications?
Yes. While most drug reactions aren’t more common in liver disease, the body can’t handle them well. A drug that causes mild liver stress in a healthy person can trigger acute injury in someone with cirrhosis. That’s why avoiding unnecessary medications is critical. Even vitamins and supplements can add up.
Is it safe to take antivirals for hepatitis if I have advanced cirrhosis?
Yes-but only with proper dosing. The TARGET-HepC study found that 22.7% of patients with Child-Pugh C cirrhosis failed treatment when given standard doses of direct-acting antivirals. When doses were adjusted, failure rates dropped to 5.3%. Always follow your liver specialist’s dosing instructions. Don’t assume the label dose is safe.
Should I get my drug levels checked regularly?
If you’re taking a drug with a narrow therapeutic index-like warfarin, digoxin, phenytoin, or tacrolimus-yes. Standard dosing can be dangerously inaccurate in liver disease. Therapeutic drug monitoring tells your doctor exactly how much drug is in your blood, so they can adjust your dose precisely. Ask your doctor if this is right for you.
Next Steps: What to Do Today
If you have liver disease:- Make a full list of every medication, supplement, and OTC drug you take.
- Bring it to your next appointment with your hepatologist or pharmacist.
- Ask: “Which of these are cleared by the liver? Do I need less?”
- Request your Child-Pugh or MELD score if you don’t already know it.
- Don’t start any new supplement without approval.
Medications aren’t one-size-fits-all-especially when your liver is damaged. The right dose isn’t what’s on the bottle. It’s what your body can handle. That’s the new standard of care.




So let me get this straight - we’re telling people with liver disease to just guess at their meds like it’s a game of Russian roulette? And the fact that 70% of prescriptions are risky? That’s not a medical guideline, that’s a public health disaster waiting for a headline.
Also, why does every single drug label still assume you’ve got a perfectly functioning liver? Like, did the FDA just forget half the population exists? I’m not mad, I’m just disappointed.
And don’t even get me started on OTC stuff. Tylenol? Sure, 2k mg/day is ‘safe’ - until it isn’t. And then you’re in the ER wondering why your ‘harmless’ headache pill turned into a liver transplant lottery ticket.
Also, why are pharmacists only now getting credit for this? They’ve been doing this work for years while doctors nodded along like they knew what they were doing. Respect to the pharmacy heroes.
And yes, I typed this on my phone. Sorry if ‘grammatically precise’ is just a fantasy I made up in my head.
Also also - if you’re taking milk thistle ‘to help your liver’ - stop. It’s not helping. It’s probably making it worse. I’m not a doctor. But I play one on Reddit.