Getting prescribed lithium for bipolar disorder means living with a tightrope. One wrong step-whether it’s popping an over-the-counter painkiller, starting a new water pill, or skipping fluids on a hot day-and your lithium levels can spike into dangerous territory. This isn’t theoretical. People have ended up in the hospital, some fatally, because of interactions that were avoidable. Lithium has a narrow window between helping and harming: 0.6 to 1.2 mmol/L. Go above that, and you risk toxicity. Below it, your mood may not stabilize. The problem? Everyday medications and simple lifestyle choices can throw this balance off completely.
How NSAIDs Turn Lithium Into a Time Bomb
NSAIDs like ibuprofen, naproxen, and even celecoxib are everywhere. People take them for headaches, arthritis, menstrual cramps. But if you’re on lithium, these drugs aren’t harmless. They interfere with how your kidneys clear lithium from your body. Normally, your kidneys filter lithium and send it out in urine. NSAIDs block the production of prostaglandins-chemicals that help keep blood flowing to your kidneys. Less blood flow means less lithium gets filtered out. It builds up. Fast.Studies show NSAIDs can increase lithium levels by 25% to 60%, depending on the drug. Indomethacin is the worst offender, often pushing levels up by 30-60%. Ibuprofen? Still risky-25-40% increase. Celecoxib is a bit safer, but not safe enough. The change doesn’t wait weeks. It happens within days. One patient might feel fine after taking ibuprofen for three days, then suddenly feel dizzy, nauseous, or confused. That’s lithium toxicity kicking in.
Older adults are at highest risk. If you’re over 65, your kidneys don’t work as well to begin with. Add an NSAID, and lithium levels can climb even faster. One case from Medsafe New Zealand involved a 72-year-old woman who took ibuprofen for joint pain. Her lithium levels rose sharply. She wasn’t monitored closely. She died. Her story isn’t rare. It’s a warning.
Diuretics: The Silent Lithium Boosters
Diuretics, or water pills, are prescribed for high blood pressure, heart failure, or swelling. But not all diuretics affect lithium the same way. Thiazide diuretics-like hydrochlorothiazide-are the biggest red flag. They cause lithium levels to rise by 25-50% within 7 to 10 days. That’s enough to push someone from safe into toxic range.Why? Thiazides make your kidneys reabsorb more sodium. Lithium rides along with sodium. So when your body holds onto sodium, it holds onto lithium too. The result? Lithium accumulates. Loop diuretics like furosemide are less dangerous, but still risky-they can raise lithium by 10-25%. And potassium-sparing diuretics like spironolactone? Their effects are unpredictable. Some studies show mild increases; others show no change. Still, it’s not worth the gamble.
Here’s the twist: some diuretics actually lower lithium levels. Osmotic diuretics like mannitol and carbonic anhydrase inhibitors like acetazolamide increase lithium excretion. That sounds good, right? Not necessarily. A sudden drop in lithium levels can trigger a return of manic or depressive symptoms. You don’t want your mood to swing because a doctor switched your water pill.
Dehydration: The Hidden Trigger
You don’t need a drug to raise lithium levels. Sometimes, all it takes is not drinking enough water. Lithium is cleared through your kidneys, and your kidneys need fluid to do their job. When you’re dehydrated-whether from sweating, vomiting, diarrhea, or just forgetting to drink-your blood volume drops. Your kidneys respond by holding onto everything, including lithium. Even mild dehydration (losing 2-3% of your body weight in water) can spike lithium levels by 15-25%.This isn’t just about hot weather. Long flights, illness, intense workouts, or even a bad stomach bug can do it. People traveling to tropical destinations or recovering from gastroenteritis are warned specifically in clinical guidelines. One patient might feel fine on lithium for months, then get the flu, stop eating, drink less, and end up in the ER with tremors, confusion, and kidney damage-all because they didn’t realize dehydration was a trigger.
Salt intake matters too. Lithium behaves like sodium in your body. If you suddenly cut back on salt-maybe you’re trying to eat healthier-your kidneys hold onto lithium to compensate. That can raise levels by 10-20%. On the flip side, eating too much salt can drop lithium levels, making your mood treatment less effective. The key? Keep your sodium intake steady. Don’t go on low-sodium diets without talking to your doctor.
Who’s Most at Risk?
Some people are walking into danger without realizing it. The highest-risk groups include:- People over 65-kidney function declines naturally with age, and they’re more likely to take NSAIDs or diuretics.
- Those with kidney disease-even mild impairment increases lithium retention.
- Patients with heart failure or low blood pressure-these conditions reduce kidney blood flow, making lithium clearance harder.
- Anyone on multiple medications-especially ACE inhibitors, SSRIs, or other drugs that affect kidney function.
- People with eating disorders or chronic vomiting/diarrhea-fluid and electrolyte loss spikes lithium levels.
One study found that patients over 65 had more than three times the risk of lithium toxicity compared to younger adults. And it’s not just about age. It’s about the combination. An elderly person on lithium, hydrochlorothiazide, and ibuprofen? That’s a perfect storm.
What to Do If You’re on Lithium
You don’t have to give up pain relief or blood pressure control. But you need a smarter plan.1. Avoid NSAIDs if you can. Use acetaminophen (Tylenol) instead for pain or fever. It doesn’t affect lithium clearance. If you must use an NSAID, take the lowest dose for the shortest time possible.
2. Never start a new diuretic without telling your doctor. If you’re on lithium and your doctor prescribes a water pill, ask: Is this a thiazide? If yes, your lithium dose may need to be lowered. Your levels must be checked within a week and again after two weeks.
3. Drink water-consistently. Don’t wait until you’re thirsty. Aim for at least 8-10 glasses a day. Increase intake during heat, exercise, or illness. Keep a water bottle with you. Set phone reminders if you need to.
4. Don’t change your salt intake. Avoid low-sodium diets unless your doctor specifically recommends it. Use salt normally in cooking and meals. Don’t suddenly go salt-free.
5. Get regular blood tests. Lithium levels should be checked every 3-6 months when stable. But after any new medication or illness, check within 7-14 days. Some clinics recommend weekly checks for the first month after starting an NSAID or diuretic.
6. Know the warning signs. Early toxicity includes diarrhea, nausea, hand tremors, dizziness, or feeling unusually tired. Later signs: blurred vision, ringing in the ears, muscle weakness, confusion. Severe cases can lead to seizures or coma. If you feel off, get your lithium level checked-don’t wait.

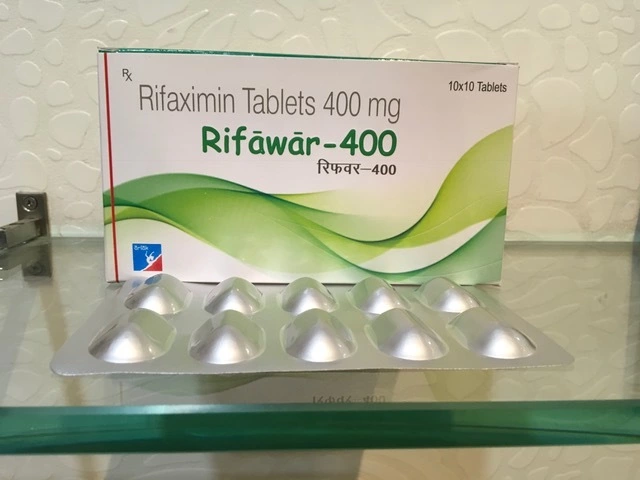
What About Herbal Diuretics?
You might think “natural” means safe. But herbal weight-loss teas, dandelion root supplements, or green tea extracts marketed as “detoxifiers” can act as diuretics. They’re unregulated, unpredictable, and dangerous with lithium. One study documented lithium toxicity in patients who took these without telling their doctors. There’s no safety data. No dosing guidelines. Just risk. If you’re using any herbal product, tell your prescriber. Even if it’s “just a tea.”Monitoring Isn’t Optional
The biggest failure in lithium care isn’t the drugs-it’s the monitoring. Many patients never get their levels checked after starting a new medication. Electronic health records often flag these interactions, but if a doctor ignores the alert-or if the patient doesn’t follow up-the system fails. One fatal case cited in Medsafe’s report happened because lithium levels were only checked “sporadically.” That’s not care. That’s luck.Good care means:
- Regular lithium blood tests-every 3-6 months, more often if anything changes.
- Immediate testing after starting or stopping any new medication.
- Communication between your psychiatrist, primary care doctor, and pharmacist.
- Patients speaking up: “I started taking this pill. Should I get my lithium checked?”
There’s still a gap in the research. Many interaction risks are based on case reports and small studies. We don’t have perfect numbers for how often toxicity happens with each combination. But we know enough to act. You don’t need a perfect study to avoid a preventable death.
Final Thoughts
Lithium saves lives. But it demands respect. It’s not a drug you can take and forget. It’s a tool that needs constant tuning-like a car that needs regular oil changes. NSAIDs, diuretics, dehydration-they’re all things that can turn that tool into a hazard. The good news? You can control most of these risks. Know your triggers. Stay hydrated. Avoid unnecessary NSAIDs. Tell your doctor about every pill you take-even the ones you think don’t matter. And never skip your blood tests. Your mood stability-and your life-depends on it.Can I take ibuprofen if I’m on lithium?
It’s not recommended. Ibuprofen can raise lithium levels by 25-40%, increasing the risk of toxicity, especially in older adults or those with kidney issues. Use acetaminophen (Tylenol) instead for pain relief. If you must take ibuprofen, use the lowest dose for the shortest time and get your lithium level checked within a week.
Do all diuretics raise lithium levels?
No. Thiazide diuretics like hydrochlorothiazide are the most dangerous, often raising lithium by 25-50%. Loop diuretics like furosemide have a smaller effect (10-25%). Potassium-sparing diuretics like spironolactone have inconsistent effects. Osmotic and carbonic anhydrase inhibitors (like mannitol or acetazolamide) actually lower lithium levels, which can cause mood instability. Always consult your doctor before starting any diuretic.
How does dehydration affect lithium levels?
Dehydration causes your kidneys to hold onto water-and lithium. Losing just 2-3% of your body weight in fluids can raise lithium levels by 15-25%. This can happen from sweating, vomiting, diarrhea, fever, or not drinking enough. Drink water consistently, especially during illness, hot weather, or travel. Don’t wait until you’re thirsty.
Should I avoid salt on a lithium regimen?
No. Reducing salt intake can cause lithium levels to rise by 10-20%. Your body uses sodium to help clear lithium. If you eat less salt, your kidneys hold onto lithium instead. Maintain a consistent sodium intake. Don’t go on low-sodium diets unless your doctor specifically advises it.
How often should lithium levels be checked?
When stable, check every 3-6 months. After starting an NSAID, diuretic, or any new medication, check within 7-14 days. After dehydration or illness, check immediately. Some guidelines recommend weekly checks for the first month after adding a high-risk drug. Always follow your doctor’s monitoring plan.
Are herbal diuretics safe with lithium?
No. Herbal products like dandelion root, green tea extracts, or weight-loss teas can act as diuretics and raise lithium levels unpredictably. They’re not regulated, and their effects aren’t studied in people on lithium. Even “natural” products can cause toxicity. Always tell your doctor about every supplement you take.
What are the early signs of lithium toxicity?
Early signs include diarrhea, nausea, vomiting, hand tremors, dizziness, increased thirst, frequent urination, and feeling unusually tired or drowsy. If you experience these, especially after starting a new medication or becoming dehydrated, get your lithium level checked right away. Delaying can lead to seizures, kidney damage, or coma.
Can lithium toxicity cause permanent kidney damage?
Yes. Severe or repeated lithium toxicity can cause lasting kidney damage, especially in older adults or those with pre-existing kidney problems. Even after recovery, some patients show reduced kidney function. That’s why prevention-through careful medication use, hydration, and monitoring-is critical.




they're watching you. every pill you take, every glass of water you drink. they want you dependent. lithium isn't medicine it's a control mechanism. NSAIDs? diuretics? dehydration? all distractions. the real poison is the system that makes you trust doctors who don't even check your levels. they don't care if you live or die. just as long as you keep coming back.
they know you read this. they know you're scared. that's the point.