When your child is scheduled for a procedure that requires sedation or anesthesia, the most stressful part isn’t the surgery itself-it’s the uncertainty. What meds will they get? When should they stop eating? Will they panic before it starts? The good news is that pediatric pre-op medications are well-studied, highly effective, and designed to make the whole experience smoother for both kids and parents. This guide breaks down exactly what you need to know, based on current clinical standards used in leading children’s hospitals like Royal Children’s Hospital Melbourne and Children’s Hospital of Philadelphia.
Why Pre-Op Medications Matter for Kids
Children aren’t just small adults. Their bodies process drugs differently. Their airways are smaller, their metabolism is faster, and their fear response is stronger. Without proper preparation, up to 60% of kids show signs of extreme anxiety before anesthesia, according to data from the American Academy of Pediatrics. That anxiety doesn’t just make the experience harder-it increases the risk of complications like vomiting, breath-holding, or even delayed recovery.
Pre-op medications are given to reduce that fear, calm the nervous system, and make the transition into sedation as smooth as possible. Studies from RCH Melbourne show that using the right premedication cuts postoperative behavioral issues-like nightmares, clinginess, or refusal to eat-by 37%. Parents report satisfaction scores jumping from 6.2 to 8.7 out of 10 when their child receives a tailored pre-op plan.
Fasting Rules: What Your Child Can and Can’t Have
Fasting isn’t just about avoiding food. It’s about preventing aspiration-when stomach contents enter the lungs during sedation. But pediatric guidelines are more flexible than adult ones because kids empty their stomachs faster.
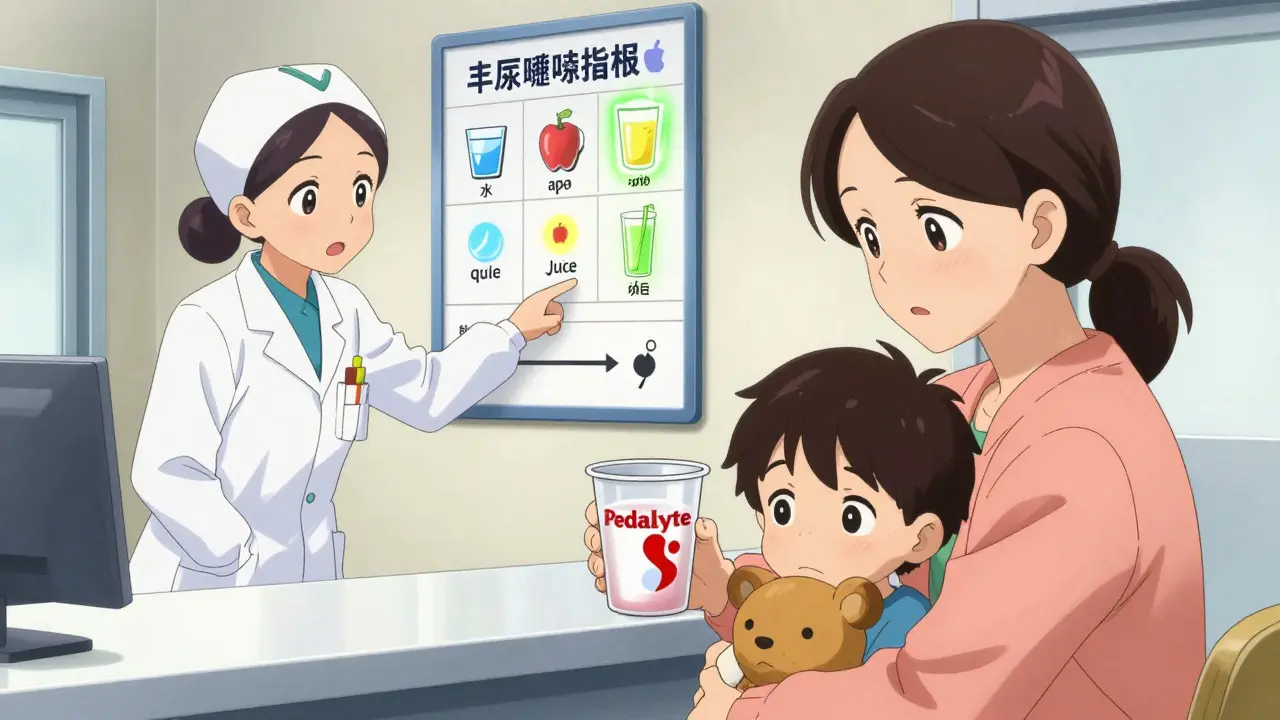
- Clear liquids (water, Pedialyte, apple juice, Sprite, 7-Up) are allowed up to 2 hours before the procedure.
- Breast milk can be given until 4 hours before.
- Milk or formula should stop 6 hours before.
- Solid foods must be avoided after midnight the night before (for children over 12 months).
Many parents get confused about what counts as a “clear liquid.” Orange juice? No-it has pulp. Milkshakes? No. Gummy candies? Absolutely not. Stick to water, electrolyte drinks, or clear sodas. If you’re unsure, call the hospital. Misunderstanding this rule is one of the top reasons procedures get delayed or canceled.
Common Pre-Op Medications and How They Work
Not every child needs medication, but for most, it’s essential. The choice depends on age, anxiety level, medical history, and the type of procedure.
Oral Midazolam
This is the most common pre-op sedative. It’s a sweet-tasting liquid given 20-30 minutes before the procedure. Dose: 0.5 to 0.7 mg per kilogram of body weight, max 20 mg. It makes kids drowsy but not unconscious. They’ll still recognize their parents, which helps with comfort.
At RCH Melbourne, nurses found that oral midazolam reduced anxiety scores by 62% on the Modified Yale Preoperative Anxiety Scale. But it doesn’t work for everyone-some kids spit it out, or it takes too long to kick in.
Intranasal Midazolam
For kids who won’t swallow pills or liquids, this spray goes into the nose. Dose: 0.2 mg per kg, max 10 mg. It works faster-about 10 minutes-and is effective in 85% of cases. Some kids get mild nasal irritation, and about 12% need an alternative. But for many, it’s the best option.
Intramuscular Ketamine
Used for highly anxious or uncooperative children, especially those with autism or developmental delays. Given as a shot in the thigh. Dose: 4 to 6 mg per kg. It creates a trance-like state where the child is calm and detached. Onset is 3-5 minutes. Parents often notice their child becomes unusually quiet or dreamy before they lose awareness. This gives time for the child to be held and comforted before full sedation.
One downside: 8-15% of kids experience emergence delirium-brief confusion or agitation when waking up. But this is manageable with gentle reassurance and usually lasts less than 10 minutes.
Special Considerations: Chronic Conditions and Medications
If your child takes daily meds, don’t stop them without clear instructions. Many parents assume all meds should be held, but that’s dangerous.
- Antiepileptic drugs (like levetiracetam, valproate): Continue as usual with a sip of water. Stopping these can trigger seizures. This is one of the most common medication errors in community hospitals.
- Proton pump inhibitors (like omeprazole) and H2 blockers (like famotidine): Keep taking them. They reduce stomach acid and lower aspiration risk.
- Asthma inhalers (albuterol): Use them as scheduled on the morning of surgery. Bronchospasm during sedation is 40% less likely when this rule is followed, according to CHOP data.
- GLP-1 agonists (like semaglutide, exenatide): These weight-loss drugs delay stomach emptying. The 2023 ASA guidance says to stop semaglutide 1 week before and exenatide 3 days before surgery.
For children with obesity, recent studies show standard midazolam doses may be too low. New guidelines suggest increasing the dose by 20% based on body weight. Always check with your anesthesiologist.
What to Expect on the Day of Surgery
Most hospitals now use a 7-step checklist to ensure safety:
- Review medical history-especially airway issues, heart conditions, or previous bad reactions to anesthesia.
- Document behavior-Is your child shy? Has autism? Has had trauma? This helps choose the right sedative.
- Reconcile medications-List every pill, inhaler, or cream your child takes. Bring the actual bottles.
- Verify fasting time-Write down when they last ate or drank. Show it to the nurse.
- Choose premedication-The team will ask if you prefer oral, nasal, or injection. Ask questions. You have a say.
- Sign consent-They’ll explain risks. Don’t rush. Ask: “What happens if we skip the sedative?”
- Check readiness-The nurse will confirm IV access, oxygen, and monitoring are in place before transport.
At RCH Melbourne, families who used this checklist reported 40% less stress. Knowing what to expect reduces fear more than any medication.

Common Mistakes and How to Avoid Them
Even in top hospitals, errors happen. Here are the top 3-and how to prevent them:
- Stopping seizure meds: 32% of medication errors involve this. Always confirm with the anesthesiologist. Never assume.
- Wrong dosing: 27% of errors are due to miscalculating weight. Bring your child’s current weight in kilograms (not pounds). Ask the nurse to double-check the math.
- Confusing clear liquids: 15% of parents think orange juice or milkshakes are okay. Stick to water, Pedialyte, or clear soda.
Also, watch for paradoxical reactions. A small number of kids (5-10%) get hyper, angry, or aggressive after midazolam instead of calm. If this happens, tell the team immediately. They have backup plans.
What Happens After the Medication?
Once the pre-op med is given, your child will likely become sleepy within 10-30 minutes. They may giggle, talk slowly, or seem out of it. This is normal. Hold them. Talk to them. Tell them you’re there. Many hospitals now let parents stay in the room until the child is fully sedated. Ask if that’s an option.
After the procedure, the effects wear off slowly. Your child may be groggy for a few hours. Don’t expect them to act like themselves right away. Some kids cry, cling, or refuse to eat. That’s not pain-it’s the sedative wearing off. Give them quiet time. Water first. Then soft foods.
Follow-up behavioral changes usually fade within 24-48 hours. If your child develops nightmares, refuses to go to the hospital again, or shows extreme fear of doctors after the procedure, talk to your pediatrician. These are rare but treatable.
Final Thoughts: You’re Not Alone
Preparing for a pediatric procedure feels overwhelming, but you’re not navigating this alone. Hospitals have teams trained specifically for this. The protocols are designed to keep kids safe, calm, and comfortable. The most powerful thing you can do is ask questions, follow the fasting rules, and trust the process.
When done right, pre-op medications don’t just make the procedure easier-they help your child feel safe, protected, and cared for. That peace of mind? It’s worth every step.





The clinical data presented here is methodologically sound, yet the omission of pharmacokinetic variance across BMI percentiles in pediatric populations remains a critical oversight. The recommended midazolam dosing (0.5–0.7 mg/kg) fails to account for adipose tissue distribution, which significantly alters volume of distribution in obese children. This is not merely a nuance-it is a clinically significant error that may lead to under-sedation and subsequent procedural failure. The 20% dose adjustment mentioned in passing lacks robust validation from prospective RCTs and should not be presented as a guideline without Level I evidence.
Furthermore, the assertion that ‘parents report satisfaction scores jumping from 6.2 to 8.7’ is statistically misleading without confidence intervals or effect size metrics. Was this a Likert scale? Was it normalized? Was there control for selection bias? These are not trivial details-they are foundational to evidence-based practice.