Managing multiple medications can feel overwhelming. You’ve got pills for your blood pressure, your diabetes, your cholesterol, maybe some pain relievers, vitamins, and herbal supplements. And you’re not sure if you’re taking them right-or even why you’re taking them. If this sounds familiar, you’re not alone. A medication action plan is your tool to take control. It’s not just a list of drugs. It’s a personalized roadmap made with your care team to help you take your medications safely, correctly, and consistently.
What Is a Medication Action Plan?
A medication action plan (MAP) is a written, patient-centered guide that tells you exactly what to do with your medications. It’s built around your life, not medical jargon. Unlike a simple prescription list, a real MAP includes specific steps: When to take each pill, why you need it, what to watch for if something goes wrong, and what to do next if you miss a dose or feel side effects. It’s not something your doctor hands you once and forgets. It’s a living document. It changes when your health changes. In Germany, since 2016, anyone taking three or more prescribed medications gets a standardized medication plan updated by their pharmacist every time they pick up a new prescription. In the U.S., Medicare Part D has required Medication Therapy Management (MTM) programs-including MAPs-for eligible patients since 2006. These plans are proven to cut hospital visits by 32% and boost adherence by up to 40%.Why Your Care Team Needs to Be Involved
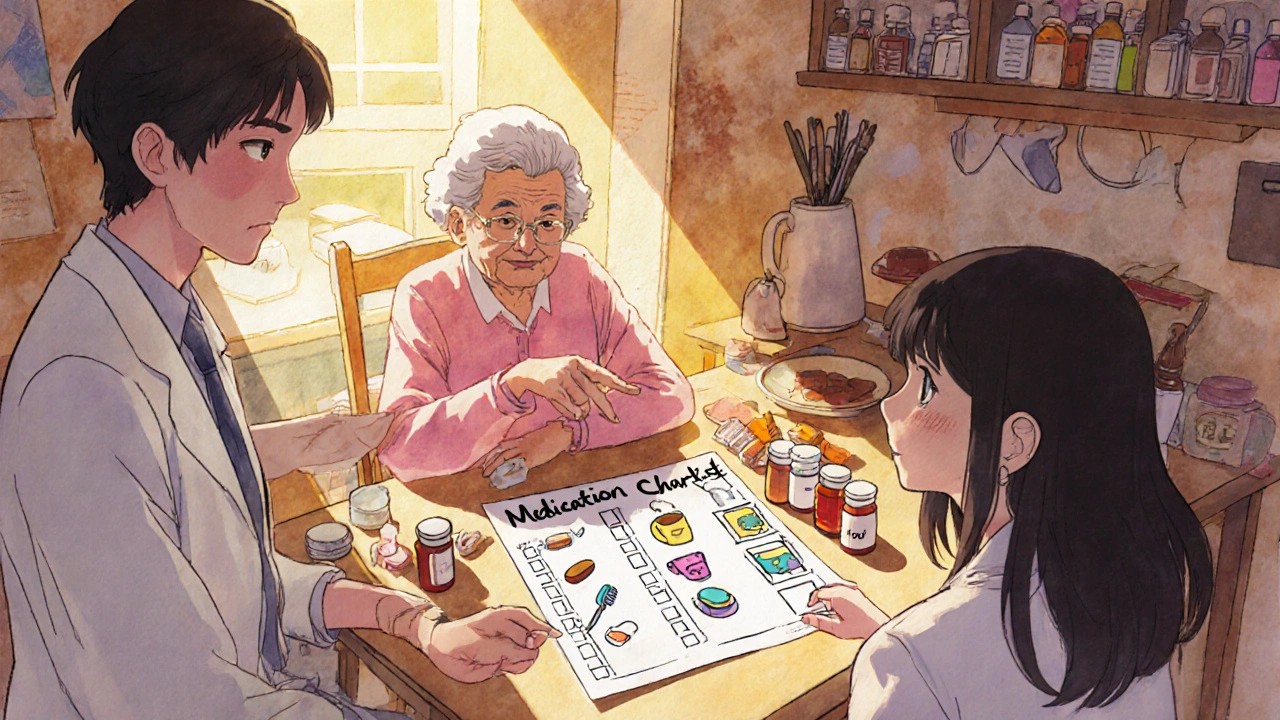
You can’t build an effective medication action plan alone. Your care team includes your doctor, pharmacist, nurse, and sometimes even a caregiver or family member. Each person brings something critical:- Your doctor knows your diagnosis, what medications are medically necessary, and how they interact with your condition.
- Your pharmacist knows every drug you take-including over-the-counter pills, vitamins, and supplements-and can spot dangerous interactions, duplications, or unnecessary prescriptions.
- Your nurse or care coordinator can help you understand how to fit your plan into your daily routine-like taking pills after breakfast or before bed.
- You know your schedule, your habits, your fears, and what makes you forget. That’s the most important part.
How to Prepare for Your Medication Action Plan Meeting
Before you meet with your care team, get everything together. Don’t rely on memory. Bring:- All prescription bottles-even the empty ones.
- All over-the-counter medicines: painkillers, antacids, sleep aids, cold pills.
- All vitamins, supplements, and herbal products (like turmeric, ginseng, or fish oil).
- A list of any recent hospital visits, ER trips, or changes in how you feel.
- Your biggest questions: “Why am I taking this?” “What happens if I forget?” “Can I stop this one?”

Building Your Plan: The 5 Key Steps
Your care team will walk through five steps with you. Don’t rush. Ask for clarification if something isn’t clear.- Reconcile your meds. Your pharmacist will compare everything you brought with what’s in your medical records. They’ll find duplicates, expired meds, or drugs you’re no longer supposed to take.
- Identify problems. Are you having side effects? Forgetting doses? Confused about timing? Running out early? These become your “medication-related problems.”
- Set goals. One goal per problem. Instead of “take my meds better,” make it specific: “Take my blood pressure pill every night at 8 p.m., next to my toothbrush, for the next 30 days.”
- Create actions. What will help you hit that goal? Use your life as the template. If you drink coffee every morning, put your morning pills next to your coffee maker. If you forget pills on weekends, use a pill organizer with days of the week. If you’re scared of side effects, write down exactly what to do: “If I feel dizzy after taking lisinopril, sit down, drink water, and call my pharmacist.”
- Plan for setbacks. What if you travel? What if you’re sick? What if you run out? Your plan should include backup steps. “If I miss a dose of warfarin, don’t double up. Call my doctor before the next dose.”
What Makes a Plan Work-or Fail
Not all plans are created equal. Here’s what separates the ones that help from the ones that gather dust:- Works: A 68-year-old woman with diabetes turned her plan into a visual chart. Each pill had a small photo next to a daily activity: coffee cup = morning meds, dinner plate = evening meds. Her adherence jumped from 65% to 95%.
- Fails: A Johns Hopkins study found patients given generic, pre-printed plans saw no improvement. Why? No personalization. No connection to their real life.
Keeping Your Plan Alive
A medication action plan isn’t a one-time thing. It’s a tool you update. Here’s how:- Review it every 3 months. Even if you feel fine, your body changes. Your meds might need adjusting.
- Update it every time you get a new prescription-or stop one.
- Take it with you to every doctor’s visit, pharmacy visit, or hospital stay.
- Share a copy with a family member or caregiver. They might notice things you miss.
- If you use a smartphone app, make sure it syncs with your plan. Many pharmacy chains now offer apps that send reminders based on your MAP.
What If Your Care Team Doesn’t Offer This?
If you’re on Medicare Part D and take 5+ chronic medications (as of 2023), you’re eligible for a free Medication Therapy Management session. Call your pharmacy or Medicare directly to ask. If you’re not on Medicare, ask your doctor or pharmacist: “Do you offer Medication Action Plans?” Many private insurers now cover them. If they say no, ask for a referral to a pharmacist who does. Community pharmacies, especially those with clinical pharmacists on staff, often provide this service-even if it’s not billed to insurance. Don’t wait for them to offer it. Be the one to ask. Your health depends on it.Real Results: Why This Matters
Medication errors cause 280,000 hospital admissions every year in the U.S. alone. Many of these are preventable. A 2022 Congressional Budget Office analysis found every $1 spent on comprehensive medication management saves $12.30 in avoided hospital stays and ER visits. But the biggest benefit isn’t money. It’s peace of mind. One Medicare beneficiary said, “I finally understood why I take each pill. I’m not just swallowing random tablets anymore.” That’s the power of a real medication action plan.What’s the difference between a medication list and a medication action plan?
A medication list just shows what drugs you take. A medication action plan tells you what to do with them. It includes when to take each pill, why you need it, what side effects to watch for, and what steps to take if you miss a dose or feel unwell. It’s personalized, action-oriented, and designed around your daily life-not just a medical record.
Can I make a medication action plan on my own?
You can start by writing down your meds and questions, but you shouldn’t create the final plan alone. Without input from your doctor or pharmacist, you might miss drug interactions, outdated prescriptions, or incorrect dosing. A care team ensures your plan is safe, accurate, and realistic for your lifestyle.
Do I need to pay for a medication action plan?
If you’re on Medicare Part D and meet eligibility (5+ chronic conditions and high medication costs), the plan is free. Many private insurers and employer plans now cover it too. Community pharmacies often offer free medication reviews-even if you don’t have insurance. Ask your pharmacist.
How often should I update my medication action plan?
Update it every time your medications change-new prescription, stopped drug, dose change. Even if nothing changes, review it every 3 months. Your body, routine, or health goals might shift. A plan that worked last month might not fit your life now.
What if my doctor and pharmacist give me different advice?
That’s a red flag. Your care team should be communicating. Ask to have a joint meeting with both your doctor and pharmacist to resolve the conflict. If they won’t coordinate, ask for a referral to a care coordinator or a pharmacy with clinical services. You deserve consistency.
Can my medication action plan help with side effects?
Yes. A good plan doesn’t just list side effects-it tells you what to do. For example: “If you feel dizzy after taking your blood pressure pill, sit down, drink water, and wait 10 minutes. If it doesn’t pass, call your pharmacist. Don’t skip the next dose.” This turns fear into a clear action, reducing panic and preventing dangerous choices.





I just threw my meds in a drawer and hope for the best. Honestly, I don’t even know what half of them are for. This post made me feel guilty, but also like maybe I should try to fix it… someday.