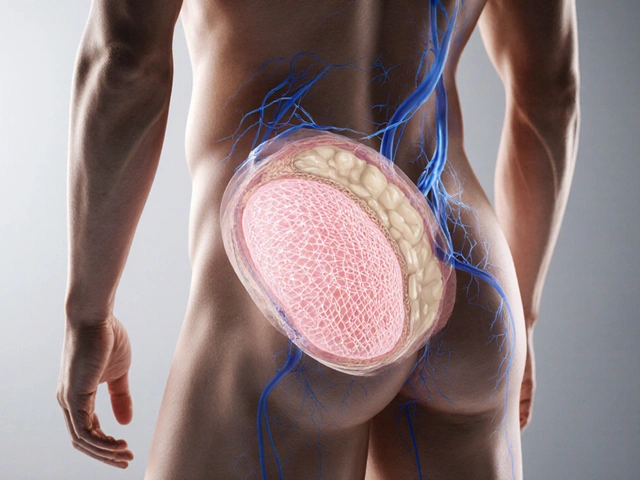
When someone says they take medication for depression or anxiety, too often the response isn’t support-it’s silence, judgment, or worse, a joke about being on drugs. This isn’t just awkward. It’s dangerous. Mental health medication stigma keeps people from getting help, causes them to skip doses, and makes them feel like they’re broken for needing treatment. The truth? Taking medication for your mental health is no different than taking insulin for diabetes or blood pressure pills for heart disease. But the stigma around it is real, widespread, and deeply rooted.
Why Mental Health Medications Are Stigmatized
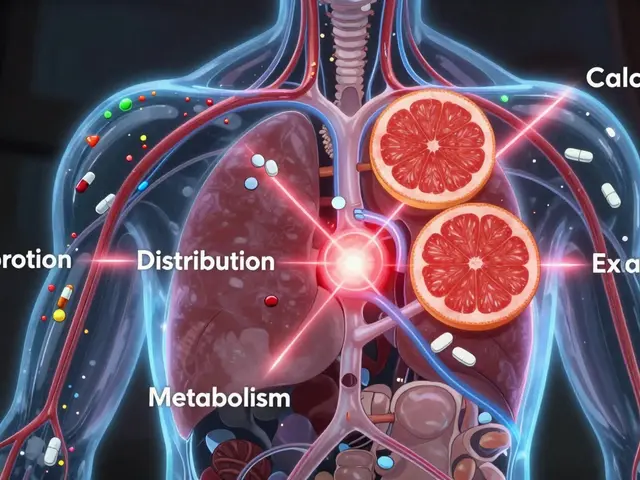
People don’t usually hate the idea of medication. They hate the idea that someone needs it for their mind. There’s a hidden belief that mental illness is a choice, a character flaw, or something you should be able to think your way out of. That’s why phrases like “just snap out of it” or “you don’t need pills” still get thrown around. And when someone admits they’re on antidepressants or antipsychotics, the reaction isn’t always empathy-it’s suspicion. Research shows that 56% of adults with mental illness don’t get treatment, and nearly one-third of them say stigma around medication is the main reason. Some believe these drugs are addictive. Others think they change who you are. A 2023 study found that 25% of people prescribed antidepressants stop taking them within 30 days-not because the medication didn’t work, but because they felt ashamed. Even healthcare providers can contribute to the problem. One study found that 22% of primary care doctors hold negative views about patients who ask for psychiatric meds. That’s not just outdated-it’s harmful. It sends the message that mental health isn’t real health.How Language Fuels the Stigma
Words matter. A lot more than you think. Say “I’m on meds” and people imagine someone popping pills at a party. Say “I take medication for my brain chemistry” and the tone shifts. The National Institute of Mental Health found that using casual terms like “pills” or “drugs” increases negative attitudes by 41%. But saying “medication,” “treatment,” or “prescribed therapy” reduces shame. It’s not about being politically correct. It’s about accuracy. Insulin isn’t a “drug” for diabetes-it’s treatment. Sertraline isn’t a “drug” for anxiety-it’s medication that balances neurotransmitters. Language shapes perception. And when we use clinical, respectful terms, we treat mental health like the medical condition it is.What Works: Proven Ways to Reduce Stigma
There are clear, research-backed ways to fight this stigma-whether you’re a patient, a provider, or someone supporting a loved one. Normalize it. Say out loud: “I take medication for my mental health, just like others take it for their heart.” That simple comparison works. Studies show that framing mental health meds as part of chronic illness management-like diabetes or asthma-reduces stigma by up to 38%. The CDC’s “Medications as Medicine” campaign used this approach in pilot communities and saw a 21% increase in positive attitudes. Educate with facts. Most people don’t know that 70-80% of people with moderate to severe depression need medication in addition to therapy to feel better. Or that antidepressants have a 40-60% success rate-comparable to many physical health treatments. When you replace myths with numbers, stigma loses its power. Use personal stories. Hearing someone say, “This medication lets me be a parent again,” or “I didn’t realize how much anxiety was holding me back until I started taking it,” changes minds more than any pamphlet ever could. A 2023 study with 700 students found that after listening to peers share their experiences, 22% more people said they’d consider medication if they needed it. Ask the right questions. If you’re a provider, don’t assume. Ask: “How do you feel about taking medication for your condition?” and “What concerns do you have?” That two-question approach increased medication adherence by 33% in one study. It shows you’re listening-not judging.
What Doesn’t Work-and Why
Not all efforts to reduce stigma actually help. Some even make it worse. For example, simulation exercises that try to make people “feel what it’s like” to have psychosis or hallucinations can backfire. A 2023 study found that when not properly explained, these experiences increased stigma by 15%. Why? Because they focus on fear, not understanding. They make mental illness feel like a horror movie, not a medical condition. Same goes for overly dramatic stories that paint mental illness as something tragic or uncontrollable. That reinforces the idea that people on medication are “broken.” The goal isn’t pity-it’s normalization. And avoid saying things like “You’re not weak for needing help.” That implies weakness is the default. Instead, say: “Taking medication is a smart, proactive step.”How Providers Can Lead the Change
Doctors, nurses, therapists-your words carry weight. Integrating mental health medication discussions into routine primary care reduces stigma. Patients don’t feel singled out when they pick up their blood pressure pills and their antidepressants at the same pharmacy. The Henry Ford Health System found that when mental health meds are managed alongside physical health care, stigma drops by 38%. Training matters too. Providers who complete 8+ hours of cultural competency training show a 29% reduction in stigma-related attitudes. Simple things-like using “medication” instead of “drugs,” or asking about side effects the same way you would for a heart medication-make patients feel seen. And don’t underestimate the power of your own story. A 2024 JAMA study found that when healthcare providers shared their own experiences with appropriate medication use (like for anxiety or depression), medical students’ stigma dropped by 37%. You don’t need to overshare. Just say: “I’ve seen how medication changes lives-for me, for my patients.”
What Patients Can Do
If you’re taking medication, you’re not alone. And you don’t owe anyone an explanation. But if you want to help break the cycle, here’s how:- Use the three-step approach: Normalize (“Many people take this”), Educate (“It helps balance brain chemistry”), Personalize (“For me, it means I can go to work without crying all day”).
- Carry your pills in a pill organizer, not a Ziploc bag. It looks like any other medication.
- When someone says, “Why do you need that?” respond with: “Why do you need your asthma inhaler?”
- Share your story with someone you trust. You might be the first person they know who’s open about it-and that can change everything.

I’ve been on SSRIs for five years now. My mom still calls them ‘chemical crutches’ - like I’m some kind of lazy bum who won’t just ‘snap out of it.’ But when I told her I take them like she takes her blood pressure meds? She shut up. Same thing. One’s for the heart, one’s for the brain. Both are organs. Both need help sometimes.
Stop treating mental health like it’s optional. You wouldn’t tell someone with diabetes to ‘just eat less sugar’ and call it a day. Why do it for depression?