Pharmacists aren’t just handing out pills anymore. In communities across the U.S., they’re giving flu shots, catching missed vaccines, and helping patients save money by switching to generic drugs-all while sitting behind the counter at your local pharmacy. This shift didn’t happen overnight. It’s the result of years of advocacy, changing laws, and real-world need. And it’s making a measurable difference in how people get care.
Pharmacists as Vaccination Champions
Right now, 93% of Americans live within five miles of a community pharmacy. That’s more accessible than any doctor’s office. Pharmacies are open late, on weekends, and without appointments. During the height of the COVID-19 pandemic, these locations became the front lines of vaccination. In the 2022-2023 flu season alone, chain pharmacies gave out over 35 million flu shots-nearly 38% of all adult flu vaccinations in the country.
It’s not just flu shots anymore. Pharmacists now administer vaccines for shingles, pneumonia, HPV, and more. In California, pharmacists can legally give any FDA-approved vaccine to anyone three years old and up. Other states have similar rules, though age limits still exist in some places, especially for kids under 12. The training isn’t easy-most pharmacists complete 20 to 30 hours of certification, including hands-on practice with injection techniques and patient counseling. But 98% of pharmacy schools now include this training in their curriculum, so new grads walk in ready to go.
Patients love it. A 2023 survey found 87% chose pharmacy vaccinations because they were convenient. No waiting rooms. No scheduling hassles. Just walk in, get the shot, and go. Pharmacists spend 7 to 10 minutes with each patient, answering questions, calming fears, and explaining why vaccines matter. On Reddit, threads show pharmacists successfully talking down vaccine-hesitant teens by breaking down mRNA science in plain language. That kind of trust doesn’t come from a hospital-it comes from consistency, visibility, and real conversation.
The Generic Prescription Advantage
While immunizations get the spotlight, pharmacists are quietly doing something just as powerful: pushing generics. A generic drug isn’t a cheaper copy-it’s the exact same active ingredient as the brand name, just without the marketing costs. Yet many patients still assume generics are inferior. Pharmacists change that.
When a doctor prescribes a brand-name medication, the pharmacist checks if a generic is available and appropriate. Then they tell the patient: “This works the same way, costs $15 instead of $120, and your insurance will cover it.” In many cases, that’s the only time the patient hears about the cheaper option. Pharmacists don’t just fill prescriptions-they educate. And that saves money. The CDC estimates that using generics saves the U.S. healthcare system over $300 billion a year.
But here’s the catch: pharmacy benefit managers (PBMs) are making it harder. These middlemen control drug pricing and reimbursement. Independent pharmacists report that 78% of them have seen PBM practices hurt their ability to offer affordable meds. Some PBMs force pharmacies to sell generics at a loss just to stay in network. Others delay payments for weeks. For small pharmacies, that’s a death sentence. And when a pharmacy closes, patients lose their most accessible health resource.
Why Payment Problems Are Holding Pharmacists Back
Pharmacists are doing more work than ever-but they’re not getting paid fairly. Medicare Part B pays only 87% of the actual cost to administer a vaccine. That means for every flu shot given to a Medicare patient, the pharmacy loses money. That’s not sustainable. Independent pharmacies, which serve rural and low-income areas, are hit hardest. They don’t have corporate backing to absorb losses.
Even when patients have insurance, billing is a mess. Forty-two percent of patients surveyed by Consumer Reports had trouble getting their pharmacy vaccination claims paid. Sometimes the pharmacy’s system doesn’t sync with the insurer’s. Other times, the insurer says the vaccine isn’t covered unless given by a doctor. Pharmacists end up spending hours on the phone, chasing payments, instead of helping patients.
The National Community Pharmacists Association has launched campaigns to fix this. They’ve gathered over 23,000 letters from pharmacists and 6,000 patient messages urging Congress to reform PBM practices. The goal? Fair reimbursement so pharmacies can keep offering these services without going broke.
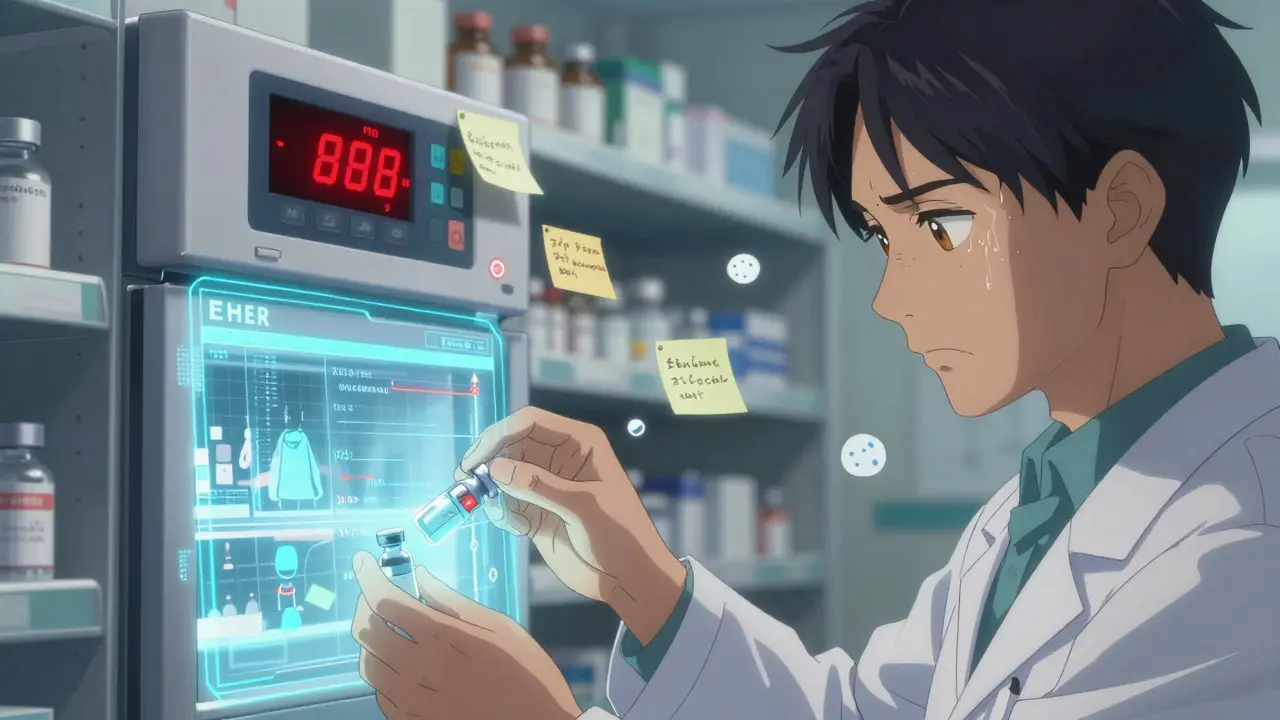
Technology Gaps and Record Keeping
Pharmacists can’t do their job well if they don’t know what vaccines a patient already got. That’s where electronic health records (EHRs) fall short. Most primary care offices don’t share vaccination data with pharmacies. And not all state immunization registries talk to each other. A patient might get a Tdap shot at the pharmacy, but their pediatrician never finds out. That leads to missed doses, duplicate shots, or worse-patients thinking they’re protected when they’re not.
The CDC says better integration is critical. A 2022 ASHP survey found 89% of pharmacists want a unified system that connects pharmacies, clinics, and hospitals. Right now, only 34 states require pharmacists to report vaccines to state registries within 72 hours. The rest have looser rules-or none at all. Without real-time data sharing, pharmacists are flying blind.
Even storage is a problem. Twelve percent of pharmacies have lost vaccines due to temperature failures. One spoiled batch can cost $1,200. That’s not just a financial hit-it’s a public health risk. Pharmacies need better refrigeration, monitoring tools, and backup power. These aren’t luxury items. They’re necessities.

What’s Next for Pharmacist Advocacy?
The trend is clear: pharmacists are becoming central to public health. By 2026, experts predict they’ll administer over half of all adult vaccines in the U.S. That’s up from 35-40% today. More states are removing age restrictions. The Inflation Reduction Act of 2022 opened new doors for Medicare reimbursement. And the CDC now lists pharmacists as “critical partners” in meeting national vaccination goals.
But progress isn’t guaranteed. Without fair pay, consistent rules, and better tech, many pharmacies won’t survive. Independent pharmacists-who make up 22% of the market-are the backbone of rural healthcare. If they’re squeezed out, the gap in access will widen.
What’s needed? Three things: standardized state laws, fair reimbursement from insurers and Medicare, and a national immunization data network. Pharmacists are ready. They’ve trained, they’ve certified, they’ve shown up during crises. Now, the system needs to catch up.
How You Can Support Pharmacist Advocacy
Patients have power too. When you get a vaccine at the pharmacy, thank the pharmacist. Ask if they offer generic alternatives for your prescriptions. If your insurance denies coverage, call your insurer and ask why. Share your experience with local lawmakers. Tell them you trust your pharmacist.
And if you’re a patient with chronic conditions-diabetes, asthma, high blood pressure-ask your pharmacist to review your meds. Many offer free Medication Therapy Management (MTM) sessions. They’ll check for interactions, simplify your regimen, and find cheaper options. That’s not just convenience. That’s care.
Pharmacists aren’t waiting for permission to help. They’re already doing it. The question is whether the system will let them keep going.
Can pharmacists give all types of vaccines?
In most states, pharmacists can give FDA-approved vaccines to adults, including flu, shingles, pneumonia, and COVID-19. Some states, like California, allow them to vaccinate children as young as three. But age limits still exist in many places for younger kids, and some vaccines require a doctor’s order. Always check your state’s rules.
Why are generic drugs cheaper but just as effective?
Generic drugs contain the same active ingredients as brand-name drugs and must meet the same FDA standards for safety, strength, and quality. They’re cheaper because manufacturers don’t spend money on advertising, branding, or recouping research costs. The result? Identical effectiveness at a fraction of the price.
Do I need an appointment to get a vaccine at the pharmacy?
No. Most pharmacies allow walk-ins. Some even let you book online through their website or app, but it’s not required. Pharmacies are designed for convenience-no waiting for a doctor’s slot, no long wait times. Just show up, and you’ll usually be seen within 15 minutes.
Why does my insurance sometimes deny coverage for pharmacy vaccines?
Some insurers have outdated rules that only cover vaccines given in doctor’s offices. Others have billing system errors or require prior authorization. Pharmacists often fight these denials, but patients can help by asking their insurer for a written explanation and filing an appeal if needed.
Are pharmacists trained to handle vaccine side effects?
Yes. All certified immunizing pharmacists are trained in recognizing and managing common reactions like fainting, allergic responses, and injection-site swelling. They keep epinephrine on hand and follow CDC guidelines for post-vaccine observation. Most patients are asked to wait 15 minutes after receiving a shot.
How can I find out if my pharmacist offers generic prescriptions?
Simply ask. When your prescription is filled, say, “Is there a generic version available?” or “Can you check if this is the most affordable option?” Pharmacists are required to offer the lowest-cost alternative unless your doctor specifically says not to substitute.