When your doctor hands you a prescription for a generic drug, what’s the first thing you think? Maybe it’s, ‘Is this going to work as well as the brand name?’ You’re not alone. Many patients wonder the same thing. But here’s the truth: the difference between a brand-name pill and its generic version isn’t in the medicine-it’s in the conversation.
Why Patients Doubt Generics-Even When Science Says Otherwise
Generic drugs are required by the FDA to contain the exact same active ingredients as their brand-name counterparts. They must meet the same strict standards for strength, purity, and performance. The bioequivalence range? 80% to 125%-meaning the body absorbs them in nearly identical ways. In reality, over 90% of all prescriptions filled in the U.S. are for generics. They save patients and the system an estimated $37 billion a year. Yet, nearly one in three patients still believe brand-name drugs are more effective. Why? It’s not because of bad science. It’s because of bad communication. A 2015 study found that over half of patients said their doctor or pharmacist never talked to them about switching to a generic. No explanation. No reassurance. Just a different-looking pill handed over at the counter. That silence speaks volumes-and not in a good way.The Power of a Simple Conversation
Research from the Journal of General Internal Medicine tracked nearly 2,000 patients and found the single biggest factor influencing whether someone accepted a generic wasn’t cost, not brand loyalty, not even past experience. It was whether their clinician had spoken to them about it. Patients who received even a brief, clear explanation were 37% more likely to stick with the generic. Not because they were convinced by data alone-but because someone they trusted told them it was safe. One patient on Reddit shared how his cardiologist spent ten minutes showing him FDA data, explaining that the generic amlodipine was chemically identical to Norvasc, and even said, ‘I take generics myself.’ That patient has been on the generic for two years with zero issues. Compare that to a Healthgrades review from someone who was handed a new pill with no context. When they got headaches, the pharmacist said, ‘Some people react to generics.’ The patient stopped taking it for three weeks. The difference? One conversation built trust. The other fed fear.What Effective Communication Actually Sounds Like
Not all explanations work. Saying, ‘We can switch you to a cheaper version,’ or ‘Let’s try this and see how it goes,’ makes patients feel like they’re being used as test subjects. Effective communication has three key parts:- Authority: Mention the FDA’s 80-125% bioequivalence standard. Patients need to know this isn’t a loophole-it’s a rigorous test.
- Confidence: Use clear, direct language. Say, ‘This generic is just as safe and effective as the brand. It’s the same medicine.’ Avoid words like ‘maybe’ or ‘try.’
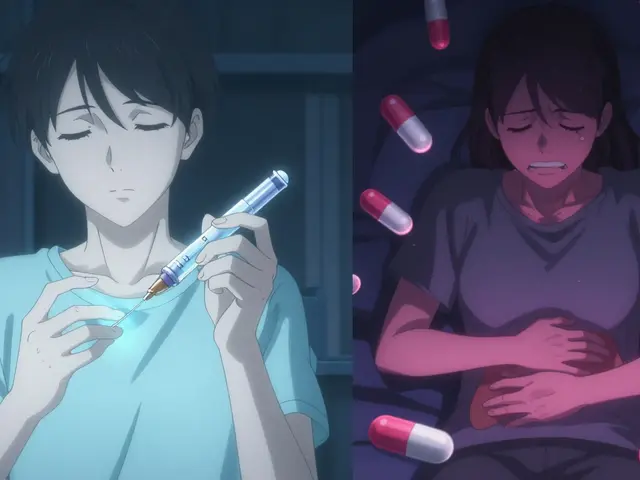
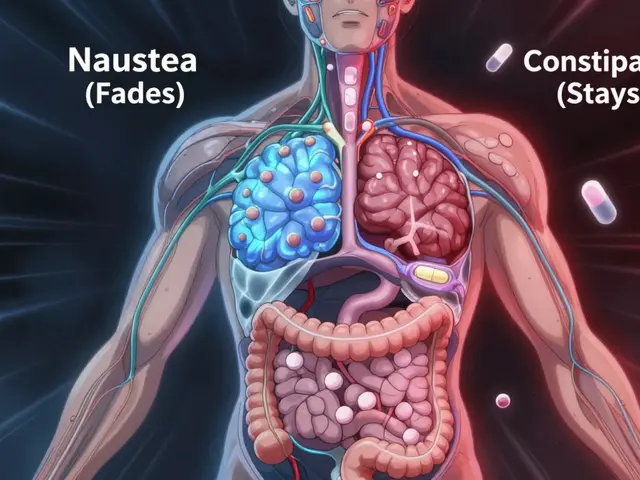
- Proactive reassurance: Address the nocebo effect. That’s when expecting side effects actually causes them. Tell patients, ‘Some people worry about changes in pills, but the medicine hasn’t changed. If you feel anything unusual, let me know-we’ll figure it out together.’
One Size Doesn’t Fit All
Communication isn’t just about what you say-it’s about who you’re saying it to. A 2016 NIH survey found non-Caucasian patients were 1.7 times more likely to doubt generics than white patients. Those with incomes under $30,000 were 2.3 times more likely to insist on brand names. These aren’t random biases. They’re shaped by history, access, and marketing. One-size-fits-all scripts don’t work. A 2021 study showed culturally competent communication-tailoring language, examples, and tone to the patient’s background-reduced skepticism by 41% in non-Caucasian groups. For some patients, showing a picture of the FDA seal helps. For others, hearing that their neighbor or family member takes the same generic makes it real. The goal isn’t to lecture-it’s to connect.Why Most Clinicians Don’t Talk About Generics-And How to Fix It
You’d think doctors and pharmacists would be the biggest advocates. But here’s the problem: - The average time spent explaining a generic switch? Just 1.2 minutes. - Only 54% of physicians could correctly explain the FDA’s bioequivalence range. - Nearly 40% of clinicians admitted they felt unsure about generics for conditions like epilepsy or thyroid disease-even though the science says they’re just as effective. Time, knowledge, and confidence gaps are real. But they’re fixable. Kaiser Permanente rolled out a ‘Generic First’ program with mandatory training, standardized scripts, and EHR prompts. Result? 94% generic utilization. $1.2 billion saved annually. The American Pharmacists Association created a 15-minute training toolkit. In a trial across 32 pharmacies, patient understanding jumped from 42% to 87%-and communication time dropped by 38%. It’s not about adding more work. It’s about doing the right thing in the right way.
The Bigger Picture: Generics Are the Future
The market for generics is growing-not shrinking. Complex generics like inhalers, injectables, and biosimilars are entering the market. These aren’t simple pills. They’re advanced therapies that need even more careful explanation. CMS now requires pharmacists to document discussions about therapeutic equivalence. Twenty-seven states have laws mandating specific communication steps. Epic Systems launched a ‘Generic Confidence Score’ in 2024 that nudges clinicians to cover key points during EHR visits. The CDC is planning to include generic communication in national health literacy standards by 2025. Medicare Part D is moving toward tying reimbursement to how well providers explain generics. This isn’t just policy. It’s a recognition: communication isn’t a side note-it’s part of the treatment.What Patients Can Do
If you’re handed a generic and feel unsure, ask:- ‘Is this the same medicine as the brand, just cheaper?’
- ‘Has the FDA approved it the same way?’
- ‘Have you prescribed this to other patients? Did it work?’
- ‘What should I watch for? And what if I feel different?’
What Clinicians Can Do
Start small. Pick one patient today and say: ‘I’m switching you to this generic because it’s been proven to work just like the brand. The FDA requires it to be identical in active ingredients and how your body uses it. It’s saved people thousands of dollars-and I’ve seen it work just as well in my own patients.’ Then pause. Listen. Answer their questions. That’s not just good communication. That’s good medicine.Are generic medications really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict standards for quality, purity, and performance. Bioequivalence testing ensures the body absorbs them in the same way-within an 80% to 125% range. Thousands of studies and decades of real-world use confirm that generics work just as well.
Why do some people feel worse after switching to a generic?
It’s often not the drug-it’s the expectation. This is called the nocebo effect. If a patient believes a generic won’t work or will cause side effects, their brain can trigger real physical symptoms. Studies show that when patients are properly informed about the equivalence of generics, reported side effects drop by nearly 30%. Clear, confident communication from clinicians can prevent this reaction before it starts.
Do pharmacists and doctors have enough training to explain generics?
Not always. A 2019 survey found only 54% of physicians could correctly explain the FDA’s bioequivalence standard. Many clinicians lack confidence, especially with complex drugs like those for epilepsy or thyroid conditions. But training programs exist. The American Pharmacists Association’s toolkit, for example, improved patient understanding from 42% to 87% in just 15 minutes of training. The issue isn’t lack of ability-it’s lack of consistent practice and support.
Can communication really save money in healthcare?
Absolutely. Generics make up 90% of prescriptions but only 23% of drug spending-saving $37 billion a year in the U.S. alone. When patients don’t accept generics due to mistrust, they often stick with expensive brand names. Studies show that effective communication can increase generic acceptance by 12-15 percentage points. That could mean an extra $180 billion in savings over the next decade. Better communication isn’t just ethical-it’s economically essential.
What should I do if my doctor doesn’t talk about generics?
Ask. Say, ‘I noticed I’m getting a different pill. Can you explain how it compares to the brand?’ or ‘Is this generic approved by the FDA the same way?’ Most clinicians appreciate patients who ask thoughtful questions. If they’re unsure, they can consult resources like the FDA’s ‘Understanding Generic Drugs’ guide or use standardized scripts from professional organizations. Your curiosity helps them do better.
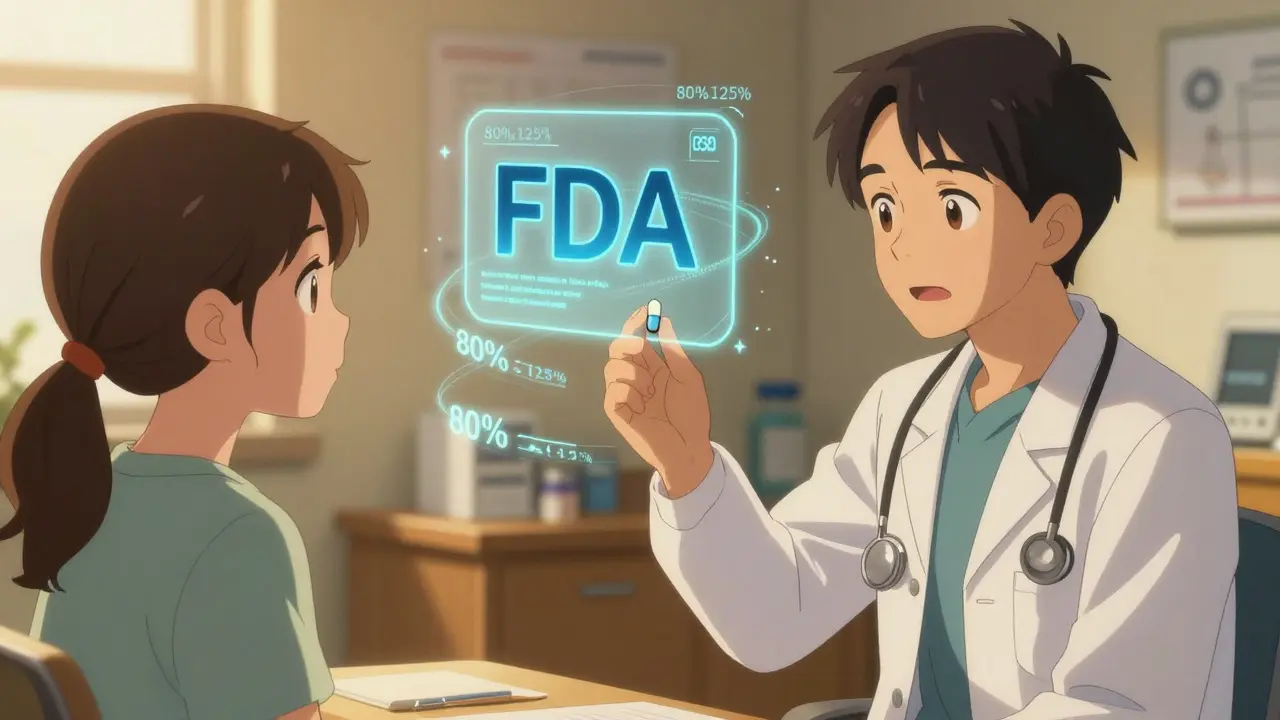



It is imperative to acknowledge, unequivocally, that the bioequivalence parameters established by the FDA-namely, the 80%–125% range-are not merely statistical conveniences; they are rigorously validated pharmacokinetic thresholds, derived from randomized, double-blind, crossover trials involving hundreds of subjects per drug formulation. The notion that generics are ‘inferior’ is a persistent myth, perpetuated by marketing, not science.
Moreover, the nocebo effect, as documented in JAMA and The Lancet, is not anecdotal-it is quantifiable. Patients who are not properly counseled exhibit statistically significant increases in self-reported adverse events, even when the pharmacological profile remains identical. This is not placebo; it is psychopharmacological priming.
The data from Kaiser Permanente and the APhA training modules are not outliers-they are replicable interventions. The 94% adoption rate and 87% comprehension spike are not magic. They are the direct result of structured, standardized communication protocols embedded in clinical workflows.
It is also worth noting that the FDA’s Orange Book explicitly lists therapeutic equivalence codes. ‘AB’ rated generics are interchangeable without clinician intervention. Yet, most prescribers remain unaware of this coding system. This is not ignorance-it is systemic neglect.
The economic argument is equally compelling: $37 billion annually is not a rounding error. It is the difference between a patient filling their insulin prescription or skipping doses. When we dismiss communication as ‘soft,’ we are, in effect, endorsing preventable morbidity.
Furthermore, the cultural dimensions of distrust-particularly among non-Caucasian and low-income populations-are not irrational. They are rational responses to historical exploitation, redlining in pharmaceutical access, and predatory marketing by brand-name manufacturers. To address this, we must move beyond scripts and engage in structural empathy.
The CDC’s forthcoming inclusion of generic communication in health literacy standards is long overdue. It should be mandatory, not optional. And reimbursement models must incentivize this-not penalize it.
Finally: if your clinician does not explain this, ask for a pharmacist consult. Pharmacists are the most underutilized resource in this equation. They are trained, accessible, and legally obligated to counsel on therapeutic equivalence. Use them.