Twenty years ago, an HIV diagnosis meant a death sentence. Today, it’s a chronic condition - one that many people manage with little to no disruption to their daily lives. The shift didn’t happen by accident. It came from decades of research, breakthroughs in drug design, and a quiet revolution in how treatment is delivered. The latest advancements aren’t just about keeping the virus under control. They’re about restoring peace of mind.
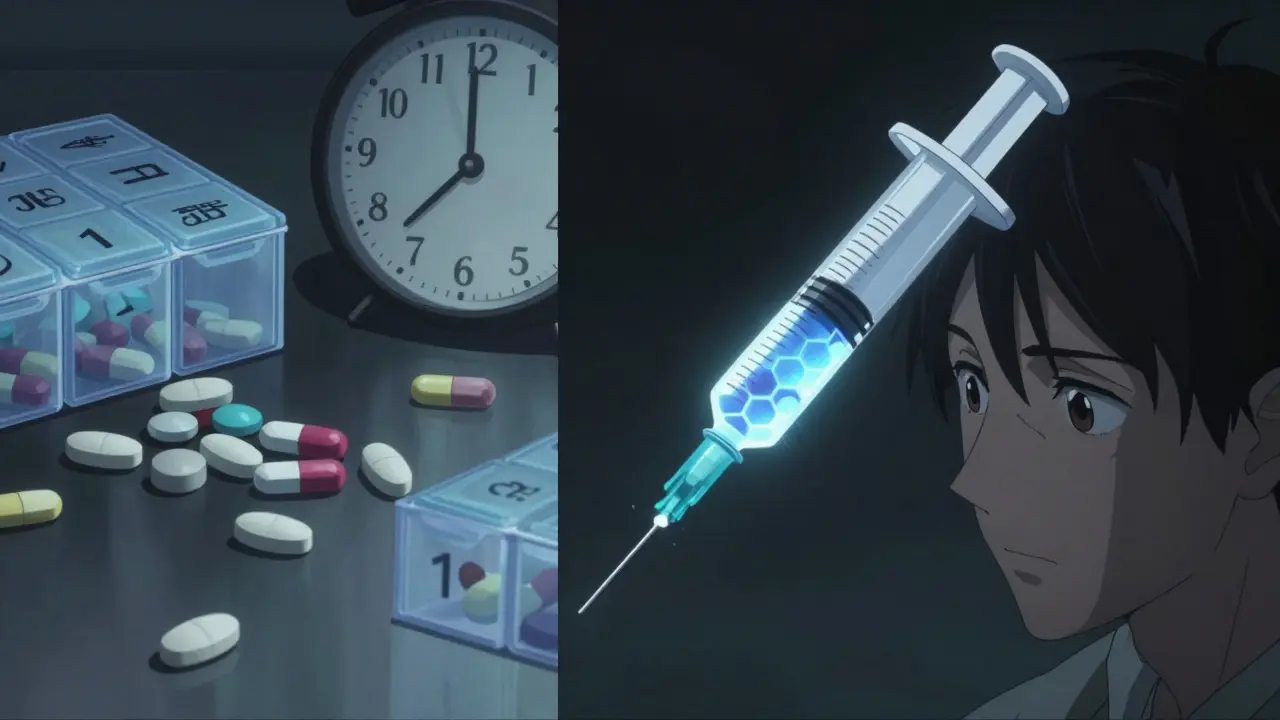
From Daily Pills to Twice-Yearly Injections
For years, the standard of care was simple: take one or more pills every single day. Miss a dose, and the virus could start replicating again. For many, this routine became a constant reminder of their diagnosis - a burden that weighed more than the pills themselves.
That changed with lenacapavir, the first capsid inhibitor approved for HIV treatment. Sold as Sunlenca, it was approved in late 2022. But what made it truly groundbreaking wasn’t just how it worked - it was how often you had to use it. A single injection under the skin lasts six months. By early 2025, that timeline got even longer.
The new LTZ regimen - combining lenacapavir with two broadly neutralizing antibodies - is now in late-stage trials and expected to be approved in mid-2026. In clinical data presented at CROI 2025, it achieved 98.7% viral suppression after 48 weeks. That’s better than daily pills. And instead of 365 doses a year, you’d need just two injections. Two. That’s it.
It’s not magic. It’s science. Lenacapavir locks onto the HIV capsid - the protein shell that protects the virus’s genetic code - and stops it from doing its job. The antibodies, teropavimab and zinlirvimab, tag the virus before it can even enter cells. Together, they create a wall the virus can’t break through. And because they’re long-lasting, your body stays protected for months.
How Modern HIV Drugs Work
HIV attacks the immune system, specifically CD4 cells. Left unchecked, it leads to AIDS - a stage where the body can’t fight off common infections. But modern antiretroviral therapy (ART) doesn’t cure HIV. It controls it. And it does so with precision.
There are seven main drug classes used today:
- NRTIs - like tenofovir and emtricitabine - trick the virus into copying itself poorly.
- NNRTIs - like doravirine - disable a key enzyme the virus needs to replicate.
- INSTIs - such as bictegravir - block the virus from inserting its DNA into your cells.
- Protease inhibitors - like darunavir - stop the virus from assembling new copies.
- CCR5 antagonists - like maraviroc - prevent the virus from entering cells by blocking a doorway.
- Fusion inhibitors - like enfuvirtide - stop the virus from fusing with your cells.
- Capsid inhibitors - lenacapavir - disrupt the virus’s protective shell.
Most people start with a single-tablet regimen. Biktarvy, for example, combines three drugs into one pill smaller than a fingernail. It’s taken once a day. No boosting. No extra pills. Merck’s DELSTRIGO is another option, especially for people with kidney issues.
But the future? It’s not in pills. It’s in injections. And the most promising one isn’t just better - it’s life-changing.
Quality of Life: More Than Just Viral Suppression
Suppression rates matter. But what really changes a person’s life isn’t the lab result. It’s the silence.
Before long-acting treatments, many people with HIV lived with constant anxiety. Would they forget their pill? Would someone see them taking it? Would they be judged? One Reddit user, u/HIVWarrior2020, wrote after switching to Sunlenca: “After 12 years of daily pills, the twice-yearly injection has eliminated my treatment-related anxiety completely.” That post got nearly 250 upvotes.
A 2025 survey of over 150,000 people using the Positive Peers app found that 92% of those on long-acting regimens rated their satisfaction as 8 out of 10 or higher. For those on daily pills? Only 76%.
The difference isn’t just emotional. It’s practical. People on twice-yearly injections are far more likely to stay on treatment. In trials, 89% of users on the LTZ regimen reported “excellent” adherence confidence. For daily pills? Just 63%.
Yes, there are downsides. Some people experience mild pain or swelling at the injection site - about 28% in one survey. But 94% said it was worth it. The discomfort lasts a day or two. The freedom lasts six months.
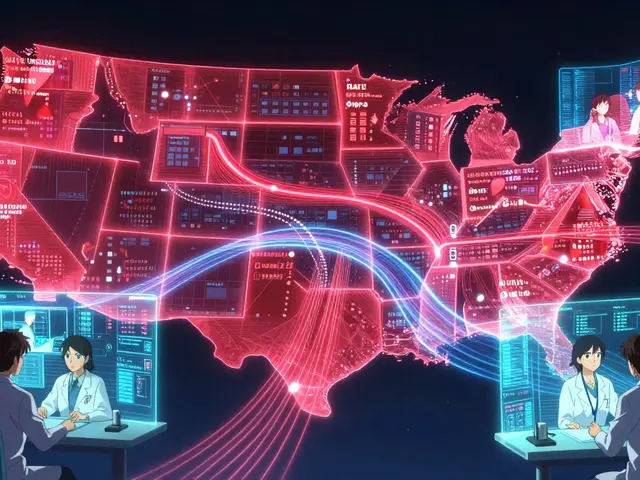
Access, Cost, and the Global Divide
Here’s the hard truth: these breakthroughs are expensive.
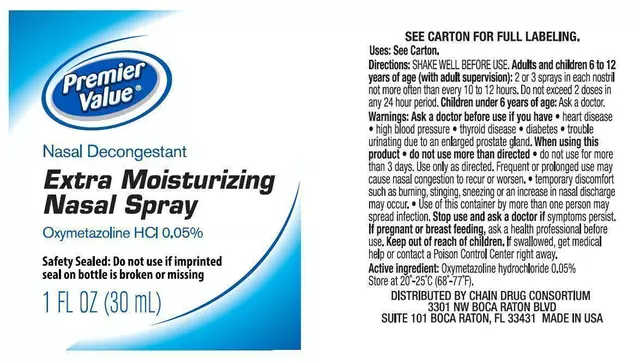
In the U.S., Biktarvy costs about $69,000 a year. Yeztugo - the same drug approved for prevention - is $45,000. That’s not sustainable. Not for individuals. Not for public health systems.
But there’s hope. A report from the European AIDS Treatment Group in October 2025 estimated that generic versions of these drugs could be produced for as little as $25 per person per year. That’s a 1,000-fold reduction. If that happens, we could cover every person who needs treatment globally - with current funding levels.
Right now, access is wildly uneven. In the U.S., 38% of people with HIV have switched to long-acting treatments. In Europe, it’s 12%. In sub-Saharan Africa - where 70% of all HIV cases live - it’s under 2%. Why? Storage. Training. Infrastructure.
Sunlenca requires cold storage: -20°C. That’s not easy in rural clinics without reliable electricity. But in June 2025, a new formulation of Yeztugo was approved with better stability. That’s a game-changer. The WHO’s July 2025 guidelines now explicitly recommend community health workers - not just doctors - administer these injections. That’s how you scale.
The real test won’t be whether the science works. It’ll be whether the world chooses to make it available to everyone.

What’s Next? The Road to 2030
By 2030, experts predict that 75% of people with HIV in high-income countries will be on long-acting regimens. In lower-income countries, that number could reach 40% - if prices drop as projected.
Other drugs are coming. ViiV Healthcare’s VH-184 and VH-499 show promise. Merck’s doravirine-islatravir combo is a once-daily two-drug option that might be safer for people with heart disease. But none match the dosing frequency of lenacapavir-based regimens.
And then there’s the bigger picture. The WHO calls lenacapavir “the next best thing to an HIV vaccine.” Why? Because when people are on effective treatment, they can’t transmit the virus. That’s not just personal health - it’s public health.
Science Magazine named lenacapavir the 2024 Breakthrough of the Year. The Warren Alpert Prize went to the scientists who made it possible. But the real winners? The people who no longer have to take a pill every day.
The end of the HIV epidemic isn’t here yet. But for the first time, we can see it - not as a distant dream, but as a reachable goal. If we act fast, if we push for fair pricing, if we train community workers and remove barriers - this could be the decade we turn the tide.
What This Means for You
If you’re living with HIV today, you have options that didn’t exist five years ago. Talk to your doctor about switching. Ask about long-acting treatments. Ask about cost assistance programs. Ask if your clinic offers them.
If you’re at risk of HIV, ask about PrEP. Yeztugo is now approved for prevention. Two shots a year. That’s it. No daily pills. No stigma. Just protection.
And if you’re not affected directly - understand this: the tools to end HIV exist. What’s missing isn’t science. It’s will.
Can HIV be cured with modern treatment?
No, modern treatments don’t cure HIV. They suppress the virus to undetectable levels, which means it can’t be transmitted and won’t damage the immune system. People on effective treatment can live long, healthy lives - but they must stay on therapy. If they stop, the virus can rebound.
How often do you need injections for long-acting HIV treatment?
Currently, Sunlenca (lenacapavir) requires two injections six months apart. The new LTZ regimen - still under review - is designed for the same schedule: just two injections per year. This is a major improvement over monthly injections like Apretude or daily pills.
Are long-acting HIV treatments available worldwide?
Not yet. They’re widely available in the U.S., Canada, and parts of Europe, but access is limited in low- and middle-income countries due to cost, storage needs, and lack of trained staff. The WHO is pushing for community health workers to administer these injections to expand access.
Can you switch from daily pills to long-acting injections?
Yes. Most people switch safely. Doctors typically overlap oral treatment with the first injection for about four weeks to ensure the virus stays suppressed. The transition is well-studied and considered safe under medical supervision.
Do long-acting HIV treatments have side effects?
The most common side effect is mild to moderate pain, redness, or swelling at the injection site - usually lasting 2-3 days. This affects about 28% of users. Serious side effects are rare. Most people find this much easier to manage than taking daily pills.
Is Yeztugo the same as Sunlenca?
Yes. Yeztugo and Sunlenca are the same drug - lenacapavir. Sunlenca is approved for treating HIV. Yeztugo is approved for preventing HIV in people at high risk (PrEP). The active ingredient and dosing schedule are identical.
How much do these treatments cost?
In the U.S., Biktarvy costs about $69,000 a year. Yeztugo is $45,000. But generic versions could be produced for as little as $25 per person per year. That’s the goal - making these life-changing treatments affordable everywhere.
Can someone on long-acting treatment still transmit HIV?
No. If the treatment is working and the viral load remains undetectable, the person cannot transmit HIV through sex. This is called U=U - Undetectable = Untransmittable. It applies to all effective HIV treatments, including long-acting ones.




Okay but let’s be real - switching to two shots a year is like going from dial-up to 5G. I used to hide my pill organizer like it was contraband. Now I just flex my arm at the clinic and call it a day. No more ‘oops I forgot’ guilt. No more ‘why are you taking medicine at lunch?’ side-eye. This isn’t treatment, it’s liberation.
Also, the fact that we’re talking about HIV like it’s just another chronic condition now? Mind blown. Twenty years ago, my cousin died in a hospice with a ‘HIV’ sticker on his door. Today? My friend got married last month. He’s got a kid. He’s got a job. He’s got two injections a year. That’s the future, folks.
And yes, I cried when I heard about the LTZ regimen. Not because I’m emotional - because it’s about damn time.