When your heart valve doesn’t open or close right, your whole body feels it. You might get winded climbing stairs, feel dizzy after walking to the mailbox, or just be tired all the time - not because you’re aging, but because your heart is fighting harder just to pump blood. This isn’t normal fatigue. It’s a sign your heart valves may be failing.
What Are Heart Valves and Why Do They Matter?
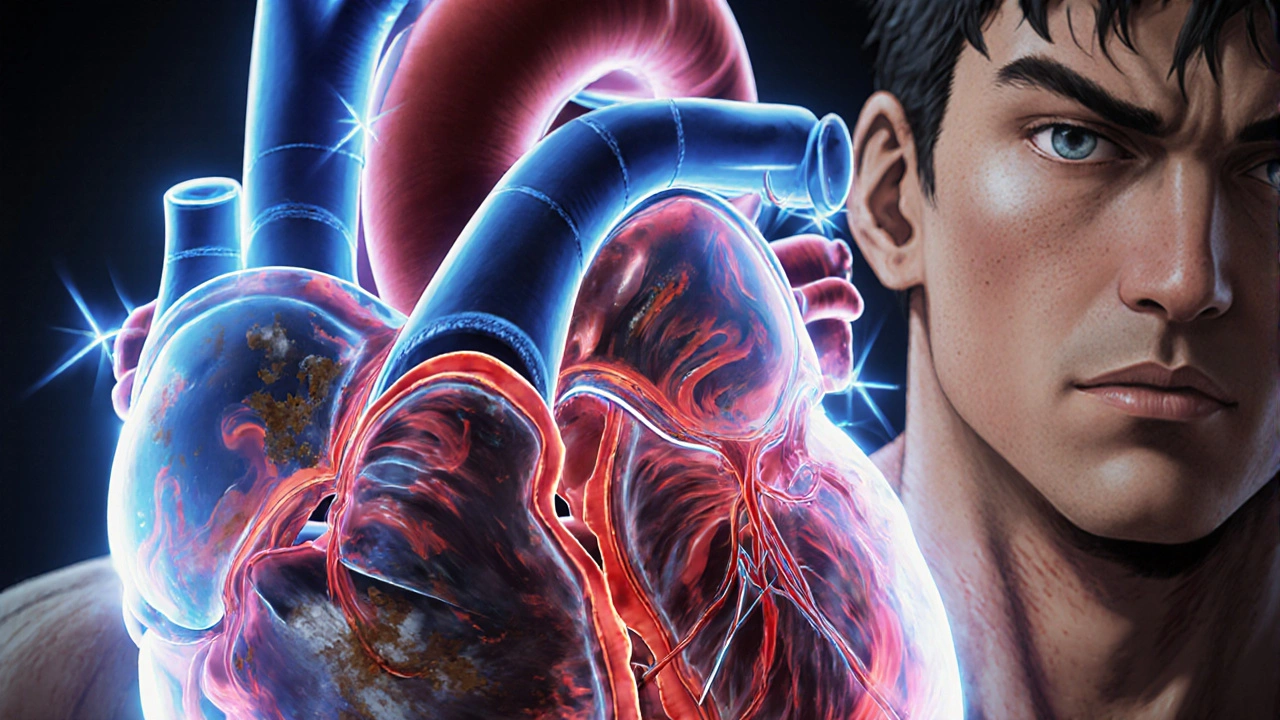
Your heart has four valves: mitral, tricuspid, aortic, and pulmonary. They’re like one-way doors that open to let blood flow forward and snap shut to stop it from leaking back. When they work right, blood moves smoothly from chamber to chamber and out to your body. But when they stiffen, narrow, or don’t seal properly, blood backs up or doesn’t get where it needs to go. That’s when valve disease kicks in.
Two main problems happen: stenosis and regurgitation. Stenosis means the valve opening gets too narrow - like a door jammed shut. Regurgitation means the valve leaks - like a door that won’t close all the way. Both make your heart work overtime. Left untreated, this can lead to heart failure, irregular heartbeats, or even sudden death.
Stenosis: When the Valve Narrows and Blocks Flow
Stenosis happens when valve leaflets thicken, calcify, or fuse together. The most common type is aortic stenosis, which affects about 2% of people over 65. In most cases, it’s caused by years of calcium buildup - not cholesterol, not diet, just aging. About half of younger patients with aortic stenosis have a bicuspid valve, a birth defect where the valve has two leaflets instead of three. It wears out faster.
Severe aortic stenosis is defined by three clear numbers: a valve area smaller than 1.0 cm², a pressure gradient over 40 mmHg, and a blood jet speed faster than 4.0 m/s. These aren’t guesses - they’re measured with echocardiograms. When these numbers hit, your heart is under serious stress. The left ventricle thickens to push blood through the tight opening. Over time, that muscle weakens. Studies show that without treatment, only half of people with severe aortic stenosis survive five years.
Mitral stenosis is less common in the U.S. but still a major issue worldwide. In developing countries, 80% of cases come from rheumatic fever - a preventable infection from untreated strep throat. The valve opening shrinks, blood backs up into the lungs, and patients struggle to breathe, especially when lying down. Severe mitral stenosis means the valve area is under 1.5 cm². At that point, even walking short distances feels impossible.
Regurgitation: When the Valve Leaks
Regurgitation is the opposite problem. Instead of being too tight, the valve is too loose. Blood flows backward, forcing the heart to pump the same blood over and over. Mitral regurgitation is the most frequent type. It can be caused by a torn chord (the strings that hold the valve in place), a stretched valve ring, or damage from a heart attack. In functional mitral regurgitation, the valve itself is fine - but the heart chamber has enlarged and pulled it out of shape.
Aortic regurgitation means oxygen-rich blood leaks back into the left ventricle after being pumped out. This causes the heart to swell and work harder to compensate. People often feel their heartbeat pounding, get short of breath during light activity, or notice swelling in their legs. Unlike stenosis, symptoms can sneak up slowly. Many patients don’t realize anything’s wrong until their heart is already enlarged.
The COAPT trial showed that for functional mitral regurgitation, a minimally invasive clip device called MitraClip reduced death and hospitalizations by 32% compared to medication alone. But for primary mitral regurgitation - where the valve is damaged - surgery gives better long-term results. Ten years after repair or replacement, survival rates are 90% versus 75% with meds only.
How Do You Know If It’s Serious?
Symptoms vary by valve and type. With aortic stenosis, the classic warning signs are chest pain, fainting, and heart failure. About 54% of patients have angina, 33% pass out, and 48% struggle with fluid buildup. But here’s the catch: many people don’t feel anything until the disease is advanced. That’s why doctors monitor asymptomatic patients with echocardiograms every 6 to 12 months. If the pressure gradient jumps above 50 mmHg, it’s time to act - even if you feel fine.
Mitral regurgitation often shows up as fatigue. One study found 79% of patients felt constantly drained, even before they noticed shortness of breath. The problem? Many doctors miss it. A 2022 survey found 28% of patients felt dismissed until they were near collapse. If you’re tired all the time and your doctor says it’s just stress, ask for an echocardiogram.
Surgical Options: Repair, Replace, or Minimally Invasive?
Not every valve problem needs open-heart surgery. Treatment depends on severity, age, overall health, and which valve is affected.
Surgical valve replacement is the gold standard for severe cases. The surgeon removes the damaged valve and replaces it with a mechanical one or a tissue valve. Mechanical valves last forever but require lifelong blood thinners. Tissue valves (from pigs or cows) don’t need anticoagulants but wear out in 15-20 years. For someone over 70, a tissue valve is usually preferred.
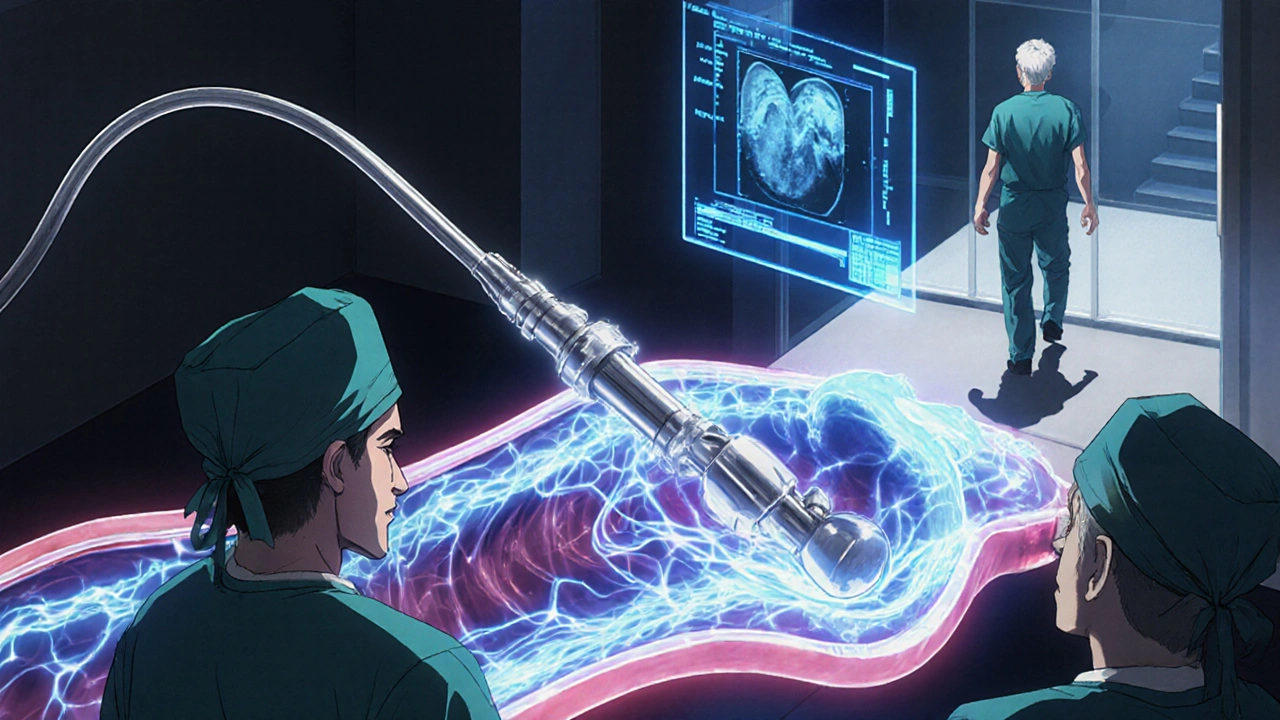
Transcatheter aortic valve replacement (TAVR) has changed everything. Instead of cracking open the chest, a new valve is threaded up through the leg artery. It’s now the first choice for patients with surgical risk scores above 4%. The PARTNER 3 trial showed TAVR cut 5-year mortality by 12.6% compared to open surgery in low-risk patients. Today, 65% of aortic valve replacements in patients over 75 are done this way.
For mitral regurgitation, MitraClip is a game-changer. It’s a tiny device that grabs the leaking edges of the valve and holds them together. No open-heart surgery. Recovery is weeks, not months. Patients report going from barely walking to hiking within two months.
For mitral stenosis, balloon valvuloplasty can stretch the valve open. It’s a 90-minute procedure with a 2-day hospital stay. It’s not permanent - the valve can narrow again - but it buys time, especially for patients who aren’t good candidates for surgery.

What Happens After Surgery?
Recovery isn’t just about healing the incision. It’s about managing your new valve. If you have a mechanical valve, you’ll need blood thinners like warfarin for life. Your INR (a blood test) must be kept between 2.0 and 3.5, depending on the valve. That means regular checks - twice a week at first, then monthly. Miss a dose, and you risk a stroke. Take too much, and you risk bleeding.
For tissue valves, you’ll need fewer meds, but you’ll need monitoring. Structural valve deterioration happens in about 21% of cases by 15 years. Newer valves are designed to last longer - some studies project 25+ years of function. But you still need yearly checkups.
Most patients report dramatic improvements. Cleveland Clinic data shows 92% of TAVR patients feel more energy within 30 days. One Reddit user wrote, “I went from struggling to walk to the mailbox to hiking 3 miles daily.” But recovery isn’t easy. Another patient said, “The sternotomy pain took 8 weeks before I could lift my grandchildren.”
What’s Next for Valve Treatment?
The future is less invasive. The FDA approved the Evoque valve for the tricuspid valve in March 2023 - the first transcatheter option for this valve. The Cardioband system and Harpoon device are in late-stage trials, aiming to repair mitral valves without replacing them. By 2030, experts predict 80% of valve procedures will be done through catheters, not open surgery.
But access isn’t equal. High-income countries perform 18 valve procedures per 100,000 people each year. Low-income nations do 0.2. That’s a 90-fold gap. Many people with rheumatic heart disease still die from preventable valve failure.
When Should You Act?
If you’re over 65 and have unexplained fatigue, shortness of breath, or dizziness - don’t wait. Get an echocardiogram. If you’re younger and have a history of rheumatic fever, heart murmur, or bicuspid valve, talk to your doctor. Valve disease doesn’t always scream for attention. Sometimes, it whispers. And if you ignore the whisper, it becomes a scream.
Early detection saves lives. Timely intervention doesn’t just add years - it adds quality. You don’t have to live with constant tiredness. You don’t have to stop walking your dog. You don’t have to wait until you’re on the brink. Your heart deserves better than that.
What’s the difference between stenosis and regurgitation?
Stenosis means the valve opening is too narrow, blocking blood flow forward. Regurgitation means the valve doesn’t close tightly, letting blood leak backward. Stenosis forces the heart to pump harder against resistance. Regurgitation makes the heart pump the same blood over and over, leading to volume overload. Both strain the heart but in different ways.
Can you live with a leaky heart valve without surgery?
Yes - for a while. Mild or moderate regurgitation often doesn’t need surgery right away. But if the heart starts enlarging, or if you develop symptoms like fatigue or shortness of breath, waiting too long can cause permanent damage. Doctors monitor these cases closely. If your ejection fraction drops or your ventricle expands, surgery becomes necessary - even if you feel okay.
Is TAVR better than open-heart surgery?
For patients over 75 or those with high surgical risk, TAVR is usually better - lower risk of stroke, shorter hospital stay, faster recovery. For younger, healthier patients, open surgery still has better long-term durability. TAVR valves can wear out faster. But newer devices are improving. The choice depends on age, overall health, and valve type.
How long do replacement heart valves last?
Mechanical valves last a lifetime but require lifelong blood thinners. Tissue valves (from animals) last 15-20 years on average, with 21% showing signs of deterioration by 15 years. Newer tissue valves may last 25+ years. For patients under 60, doctors often recommend mechanical valves. For those over 70, tissue valves are preferred to avoid blood thinners.
Can lifestyle changes fix a bad heart valve?
No. Diet, exercise, and quitting smoking won’t reverse stenosis or regurgitation. But they can help your heart handle the stress better. Managing blood pressure, avoiding infections (like endocarditis), and staying active within your limits improve outcomes. Still, if the valve is severely damaged, only repair or replacement will fix the problem.
Why do some people get diagnosed late?
Because symptoms are vague. Fatigue, shortness of breath, and dizziness are often blamed on aging, stress, or being out of shape. Doctors may not hear a murmur if they don’t listen carefully. Echocardiograms aren’t routine unless symptoms are obvious. Many patients report being dismissed until they were near collapse. If you suspect something’s wrong, push for an echo - it’s quick, painless, and life-saving.
Heart valve disease doesn’t have to be a death sentence. With modern tools, we can fix it before it breaks you. The key is knowing when to look - and when to act.


So let me get this straight - you’re telling me my grandpa’s ‘just getting old’ fatigue is actually his heart valves throwing a tantrum? 🤯 I thought he was just mad we didn’t visit enough.