Grapefruit Medication Interaction Checker
Check Your Medication
Select your prescription medication to see if grapefruit juice affects it
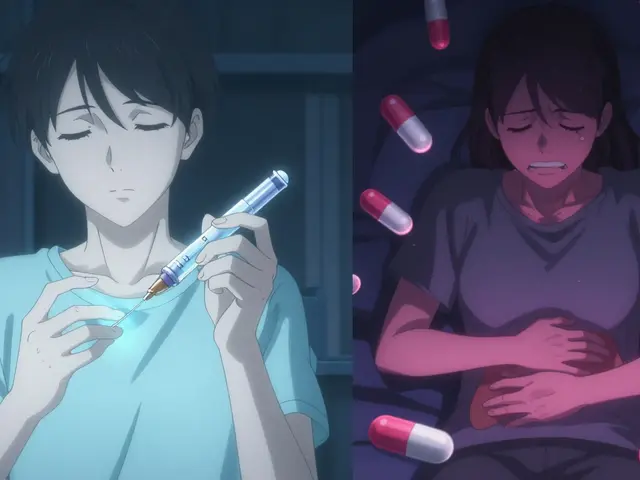
One small glass of grapefruit juice in the morning might seem harmless-maybe even healthy. But if you’re taking certain medications, that glass could be putting your life at risk. It’s not about too much sugar or too many calories. It’s about something invisible: a chemical reaction inside your body that turns a common fruit into a dangerous companion for your pills.
Back in 1989, researchers in Canada were studying how alcohol affected a blood pressure drug called felodipine. They expected some changes. What they found shocked them: grapefruit juice made the drug’s concentration in the blood jump by over 350%. That’s not a typo. It wasn’t a fluke. Since then, we’ve learned this isn’t just about one drug or one fruit. It’s a pattern that affects dozens of medications, especially in older adults who take multiple prescriptions every day.
How Grapefruit Changes Your Medication
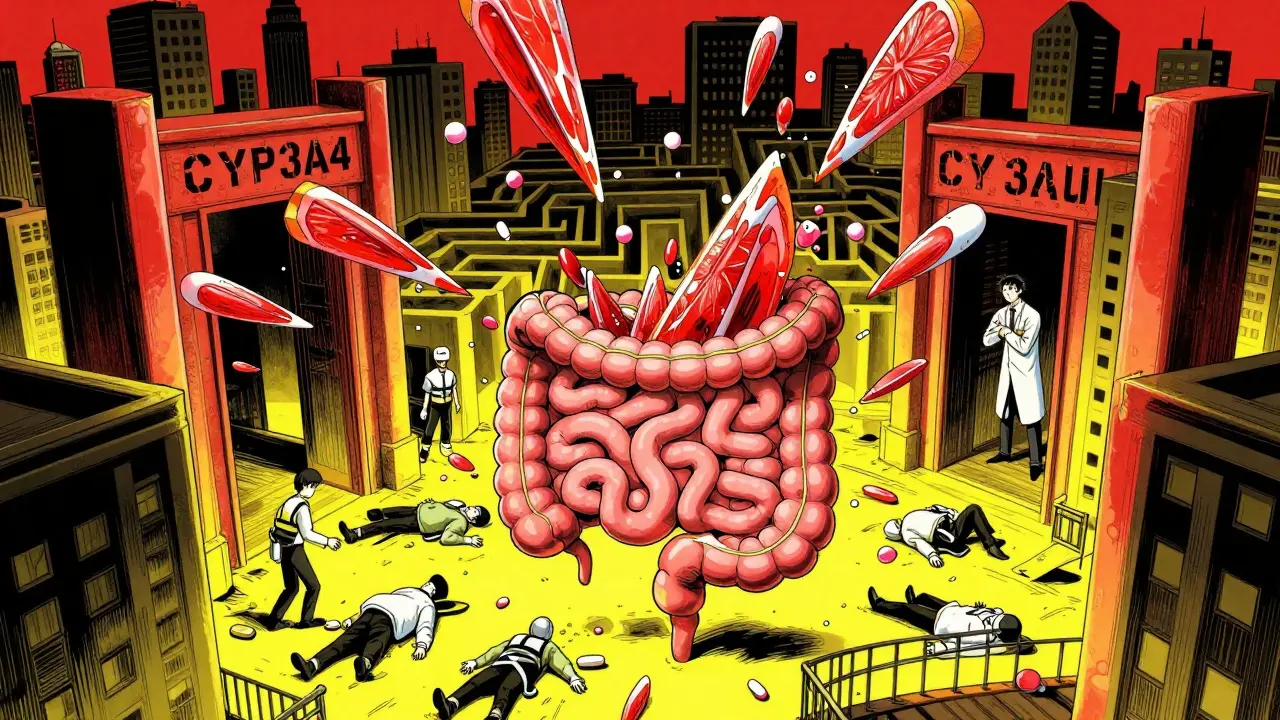
Grapefruit doesn’t just make your meds stronger-it makes them unpredictably stronger. The culprit isn’t sugar or acid. It’s a group of chemicals called furanocoumarins, mainly bergamottin and 6’,7’-dihydroxybergamottin. These compounds wreck a key enzyme in your gut called CYP3A4.
This enzyme normally breaks down drugs as they pass through your intestines before they reach your bloodstream. Think of it like a bouncer at a club-only letting in a certain number of molecules. When grapefruit juice shows up, it knocks out the bouncer. Suddenly, way more drug gets through. Your body ends up with 30% to 300% more medication than it should. And because the enzyme doesn’t just take a nap-it gets permanently disabled-you can’t just wait a few hours. The damage lasts 24 to 72 hours. One glass of juice today can affect your meds tomorrow… and the day after.
Which Medications Are Most at Risk?
Not all drugs are affected the same way. Some barely notice grapefruit. Others? They go from safe to dangerous in minutes. Here are the biggest offenders:
- Statins (cholesterol drugs): Simvastatin (Zocor) is the worst. Just 200 mL of grapefruit juice-a little over half a cup-can triple your blood levels. That raises your risk of rhabdomyolysis, a life-threatening muscle breakdown that can fry your kidneys. Lovastatin (Mevacor) isn’t far behind. Atorvastatin (Lipitor) sees an 80% spike. But pravastatin (Pravachol) and rosuvastatin (Crestor)? They’re safe. Why? Because they don’t rely on CYP3A4 to break down.
- Calcium channel blockers (blood pressure meds): Amlodipine (Norvasc) jumps 150%. Nifedipine (Procardia) shoots up 274%. Felodipine (Plendil)? Remember that 355% increase from 1989? Still true today. These drugs are meant to gently relax blood vessels. Too much? You could drop your blood pressure dangerously low.
- Immunosuppressants: These are the most dangerous. If you’ve had a transplant, grapefruit could be deadly. Cyclosporine (Sandimmune) levels rise 50-60%. Tacrolimus (Prograf) can spike 300-500%. Sirolimus (Rapamune)? A single glass can make your levels jump 1100%. That means severe kidney damage, high blood pressure, or serious infections.
- Other high-risk drugs: Some anti-anxiety meds (like buspirone), certain heart rhythm drugs (amiodarone), and even some cancer treatments (like sunitinib) are on the list. Even some erectile dysfunction drugs (like tadalafil) can become too potent.
The FDA now requires warning labels on 17 prescription drugs because of grapefruit. Another 23 have warnings in their prescribing info. That’s not a small number. That’s a public health signal.
What About Other Citrus Fruits?
It’s not just grapefruit. Seville oranges (the kind used in marmalade), pomelos, and even some limes have the same chemicals. If your orange juice tastes bitter, it might be one of these. Regular sweet oranges? Safe. Tangerines? Safe. Lemons? Safe. The difference is in the furanocoumarins-and they’re not in all citrus.
And it gets weirder. Pomegranate juice? One case study suggested it might do the same thing. No solid proof yet, but if you’re on a high-risk drug, better to skip it. Same goes for starfruit and some herbal supplements like St. John’s Wort-though that’s a different mechanism.
Why Older Adults Are at Higher Risk
You might think this only matters if you’re young and healthy. Actually, it’s the opposite. People over 65 are the most vulnerable. Why?
- They’re more likely to take 5 or more prescriptions daily. CDC data from 2021 shows over half of Americans 65+ do.
- They’re more likely to eat grapefruit. The National Health Survey found 42.7% of seniors consume grapefruit products weekly.
- Their bodies break down drugs slower. Liver and kidney function decline with age, so even small changes in drug levels can pile up.
- They’re less likely to know about the risk. A 2022 Harvard study found most older adults never heard of this interaction.
That’s why doctors and pharmacists now screen for it. In fact, 78.4% of community pharmacists in the U.S. check for grapefruit interactions during routine medication reviews. If you refill a prescription and they ask, “Do you drink grapefruit juice?”-they’re not being nosy. They’re saving your life.
What Should You Do?
Here’s the bottom line: if you take any of these medications, don’t risk it.
- Avoid grapefruit entirely. No juice, no fruit, no smoothies. Even small amounts matter.
- Check your meds. Look at the bottle. If it says “Do not take with grapefruit,” follow it. If you’re unsure, ask your pharmacist.
- Ask about alternatives. For statins, switch to pravastatin or rosuvastatin. For blood pressure meds, diltiazem or verapamil are safer options. For immunosuppressants, your doctor may be able to switch you to a non-interacting version.
- Ask three questions: Does my specific drug interact with grapefruit? How much, if any, can I safely consume? What other foods or juices should I avoid? The FDA says this is the best way to stay safe.
And if you love grapefruit? You don’t have to give up fruit. Swap it for oranges, apples, or berries. The health benefits are still there-without the hidden danger.

What’s Being Done About It?
Science hasn’t stopped here. Hospitals now have electronic alerts built into their systems. Over 90% of U.S. hospitals using Epic EHR software flag grapefruit interactions when a doctor writes a prescription. Researchers are testing modified grapefruit varieties with 85-90% less furanocoumarin. Early results are promising. But until those are widely available? The American Heart Association says: complete avoidance is still the only safe choice.
Even genetic differences matter. Some people carry a gene variant (CYP3A4*22) that makes them extra sensitive to grapefruit. Their drug levels spike 40% higher than others. That’s why blanket advice doesn’t always work-but avoidance does.
Final Reality Check
There’s no magic number. No safe amount. No timing trick. Grapefruit doesn’t just make your meds stronger-it makes them toxic in ways you can’t feel until it’s too late. Muscle pain? Nausea? Dizziness? Those aren’t side effects. They’re warning signs.
And this isn’t theoretical. The FDA estimates grapefruit interactions cause around 10,000 adverse events in the U.S. every year. Many end in hospitalization. Some end in death.
If you’re on medication, and you like grapefruit, don’t gamble. Talk to your doctor. Talk to your pharmacist. Get the facts. Because sometimes, the healthiest thing you can do is skip the fruit altogether.
Can I just drink grapefruit juice a few hours before or after my medication?
No. The enzyme inhibition from grapefruit lasts 24 to 72 hours. Even if you take your pill in the evening and drink juice in the morning, the enzyme in your gut is still disabled. Timing doesn’t help. Avoidance is the only reliable strategy.
Are all grapefruit products equally dangerous?
Yes. Whether it’s fresh fruit, juice, frozen pulp, or even flavored water with grapefruit extract, they all contain the same furanocoumarins. Even small amounts-like a splash in a smoothie-can trigger an interaction. There is no "safe dose" for high-risk medications.
I take a statin. How do I know if mine is affected?
Simvastatin and lovastatin are high-risk. Atorvastatin has a moderate risk. Pravastatin and rosuvastatin are safe. Check your prescription label or ask your pharmacist. If you’re unsure, get the generic name-it’s easier to look up.
What if I can’t live without grapefruit juice?
Ask your doctor if there’s an alternative medication that doesn’t interact. For statins, pravastatin or rosuvastatin work just as well. For blood pressure, diltiazem or verapamil are safer. For immunosuppressants, your doctor may switch you to a non-CYP3A4-dependent drug. Your health is worth the change.
Does grapefruit affect over-the-counter drugs?
Yes. Some OTC antihistamines (like fexofenadine) and sleep aids (like diphenhydramine) can be affected. Even some herbal supplements like St. John’s Wort. Always check the label or ask your pharmacist before mixing anything with grapefruit.