What Really Causes GERD and Acid Reflux?
GERD isn’t just occasional heartburn after a spicy meal. It’s when your stomach acid keeps leaking back into your esophagus-often enough to cause real damage. The problem starts with the lower esophageal sphincter (LES), a ring of muscle that should act like a one-way valve. When it weakens or relaxes at the wrong time, acid rises up. That’s when you feel that burning chest pain, the sour taste in your mouth, or even a chronic cough.
Studies show that 90% of people with GERD report heartburn as their main symptom. But it’s not just about discomfort. Left untreated, chronic acid exposure can lead to esophageal strictures, ulcers, or even Barrett’s esophagus-a precancerous condition that affects 10-15% of long-term GERD patients. The good news? Most cases respond well to the right mix of lifestyle changes and medication.
Why Lifestyle Changes Are the First Step
Doctors don’t start with pills for a reason. Lifestyle changes are the most effective first-line treatment for GERD-and they work for most people. The key isn’t perfection; it’s consistency.
Weight loss is one of the biggest game-changers. If you’re overweight, losing just 5-10% of your body weight can cut your symptoms in half. That’s not magic-it’s physics. Extra belly fat pushes up on your stomach, forcing acid out. A 2022 study found that people who lost weight saw a 70% drop in nighttime reflux episodes.
Timing matters too. Eating within two or three hours of lying down doubles your risk of acid rising into your esophagus. Try finishing dinner by 7 p.m. if you go to bed at 10. Elevating the head of your bed by 6 inches (using blocks or a wedge pillow) can also help gravity keep acid where it belongs.
Trigger foods aren’t the same for everyone, but some are nearly universal. Coffee, tomatoes, alcohol, chocolate, and fatty or spicy foods make symptoms worse in 70-80% of people. Cutting out just coffee alone helped 73% of users in one survey. Keep a simple food diary for two weeks. Write down what you eat and when symptoms hit. You’ll likely find your own personal triggers faster than you think.
How PPIs Actually Work (And Why They’re So Popular)
Proton pump inhibitors-PPIs like omeprazole, pantoprazole, and esomeprazole-are the most powerful acid-reducing drugs available. They don’t just calm things down; they shut off the acid production at its source. While antacids give quick but short relief, and H2 blockers like famotidine cut acid by about 60%, PPIs reduce stomach acid by 90-98%.
That’s why they’re so effective at healing esophagitis. Clinical trials show PPIs heal inflammation in 70-90% of patients within 8 weeks, compared to just 50-60% with H2 blockers. They’re the go-to for anyone with confirmed erosive esophagitis or frequent, severe symptoms.
But timing is critical. PPIs work best when taken 30-60 minutes before your first meal of the day. Taking them after eating? You’re wasting half their power. And don’t double up unless your doctor says so. More isn’t better-it just increases side effect risk.
The Hidden Costs of Long-Term PPI Use
PPIs work too well for some people to stop. But using them for more than a year can come with real risks. The FDA has issued warnings about increased fracture risk in older adults taking high doses for three years or more. Studies also link long-term PPI use to a 20-50% higher chance of intestinal infections like C. diff, vitamin B12 deficiency, and kidney inflammation.
And here’s something many don’t know: stopping PPIs suddenly can cause rebound acid hypersecretion. Your stomach, used to being quiet, goes into overdrive. Symptoms get worse for a few weeks-even if your GERD was under control. That’s why people think the drug “stopped working,” when really, their body just reacted to the sudden change.
One study found 44% of users experienced this rebound effect. The fix? Taper slowly. Switch to an H2 blocker like famotidine for a few weeks while gradually reducing your PPI dose. This gives your stomach time to readjust without the painful spike.
What Works Better Than PPIs Alone
Some patients do great on PPIs. Others? They get side effects-headaches, diarrhea, low magnesium-and still don’t feel better. That’s where combining approaches makes the difference.
A 2023 study from Johns Hopkins tracked patients who followed a 12-week lifestyle program: weight loss, trigger food elimination, and bedtime fasting. Half of them were able to stop PPIs completely-and kept their symptoms under control. That’s double the success rate of those who just kept taking pills.
One patient from Melbourne shared her story: after years of PPIs and no relief, she started sleeping with her head elevated and cut out coffee and chocolate. Within three weeks, her nighttime cough vanished. She’s now off PPIs for 18 months.
Even small changes add up. One study showed that combining bed elevation with dietary changes reduced nighttime reflux by 60%. That’s more than most medications can do alone.
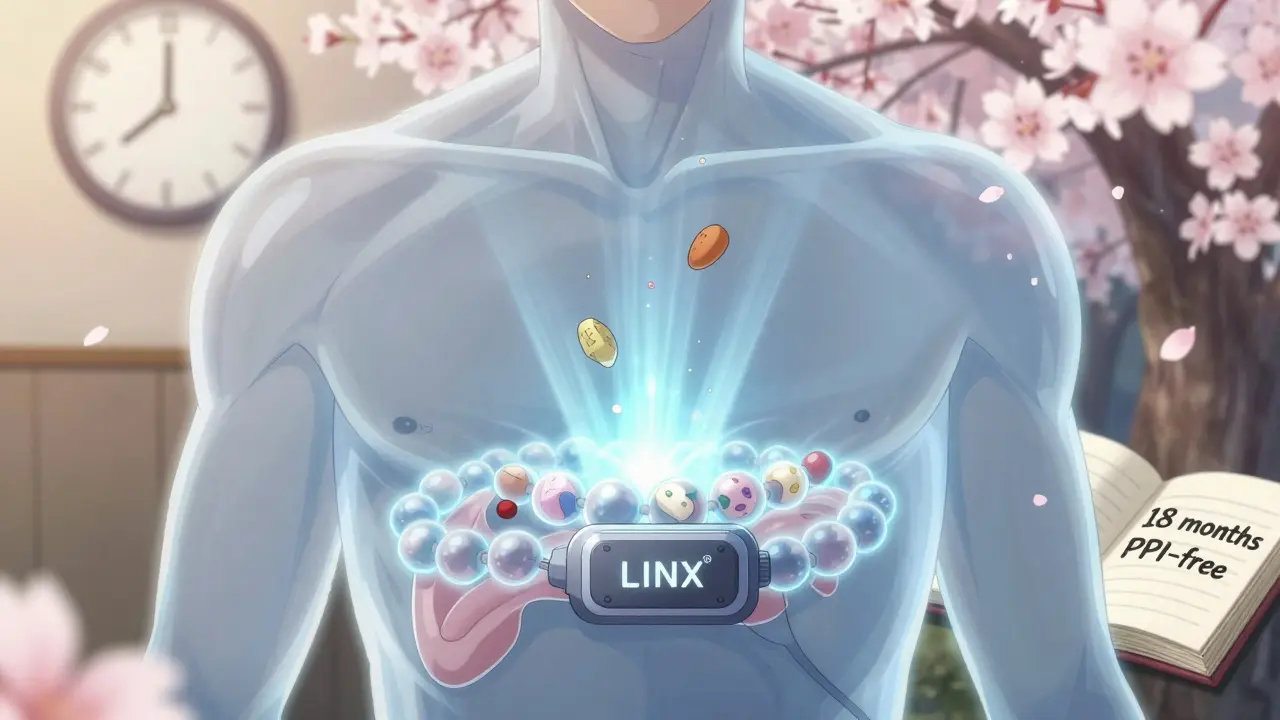
When to Think About Surgery
Surgery isn’t the first option-but it’s a solid one if things don’t improve. For people who can’t tolerate PPIs, don’t respond to them, or want to avoid lifelong meds, fundoplication (a procedure that wraps the top of the stomach around the LES) has a 90% success rate at 10 years.
Newer options like the LINX® device-a ring of magnetic beads placed around the LES-let food pass normally but prevent acid from rising. Five years after implant, 85% of patients report major symptom improvement. And procedures like TIF (transoral incisionless fundoplication) are gaining traction because they’re less invasive and have high patient satisfaction rates.
But surgery isn’t for everyone. It’s usually reserved for those with confirmed anatomical issues like a hiatal hernia, or those who’ve tried everything else. Your doctor will need to run tests-like an endoscopy or pH monitoring-to see if you’re a candidate.
How to Know If You’re on the Right Path
Feeling better doesn’t mean you’re healed. Many people stop PPIs once their heartburn fades-but the inflammation in their esophagus might still be there. That’s why doctors recommend a full 8-week course, even if you feel fine after two weeks.
Watch for red flags: trouble swallowing, unexplained weight loss, vomiting blood, or black stools. These aren’t normal GERD symptoms. They could mean strictures, ulcers, or worse. Get an endoscopy if they show up.
Regular check-ins matter too. The American College of Gastroenterology recommends reevaluating PPI use every 8 weeks. Ask yourself: Do I still need this? Can I lower the dose? Could I switch to an H2 blocker on an as-needed basis?
Tools That Actually Help
Managing GERD is easier with the right support. Apps like RefluxMD let you log meals, symptoms, and sleep position. With 8,500 users and a 4.7/5 rating, it helps spot patterns you’d miss on paper.
Organizations like the International Foundation for Gastrointestinal Disorders offer free, evidence-based guides on diet, medication, and coping strategies. And if you’re in Australia, local dietitians often have GERD-specific meal plans tailored to local foods.
Don’t underestimate the power of community. Reddit’s r/GERD has over 100,000 members sharing what worked (and what didn’t). You’re not alone in this.
What’s Next in GERD Care
The field is changing fast. In 2023, the FDA approved Vonoprazan-a new type of acid blocker that works faster and more reliably than PPIs in some patients. Early trials show 89% healing rates in erosive esophagitis.
AI-powered food diaries are being tested to predict your personal triggers with 78% accuracy. Imagine your phone telling you, “You had pasta at 7 p.m. and felt heartburn at 10 p.m. Try eating earlier next time.”
But the biggest shift? Moving away from automatic PPI prescriptions. New guidelines from the American Gastroenterological Association now say lifestyle changes should come first-every time. PPIs are for confirmed cases, not guesses.
Final Takeaway: It’s Not Either/Or
GERD doesn’t have to be a life sentence of pills or pain. The most successful people aren’t the ones who took the strongest drug-they’re the ones who combined smart habits with smart medicine.
Start with lifestyle: lose a little weight, avoid late-night meals, cut your biggest triggers. Give it 4-6 weeks. If symptoms persist, talk to your doctor about PPIs. But don’t assume you’ll need them forever. Reassess every few months. Ask about stepping down. Use tools to track progress.
GERD is manageable. Not because of one miracle fix-but because of consistent, smart choices.





Life isn't about fighting acid it's about listening to your body
Stop treating symptoms like enemies and start seeing them as whispers
That burn? It's your soul asking for space
That cough at night? It's your body screaming for stillness
You don't need more pills you need more peace
Eat when the sun is high sleep when the moon is low
Let your rhythm be your remedy