Most people with gallstones never know they have them. But for those who do, the pain hits like a sledgehammer-sharp, steady, and stuck in the right side of the belly, often after a fatty meal. It doesn’t go away with gas or vomiting. It just hangs on for hours, then fades, only to come back days or weeks later. This isn’t just bad digestion. This is biliary colic, the first warning sign that gallstones are causing trouble.
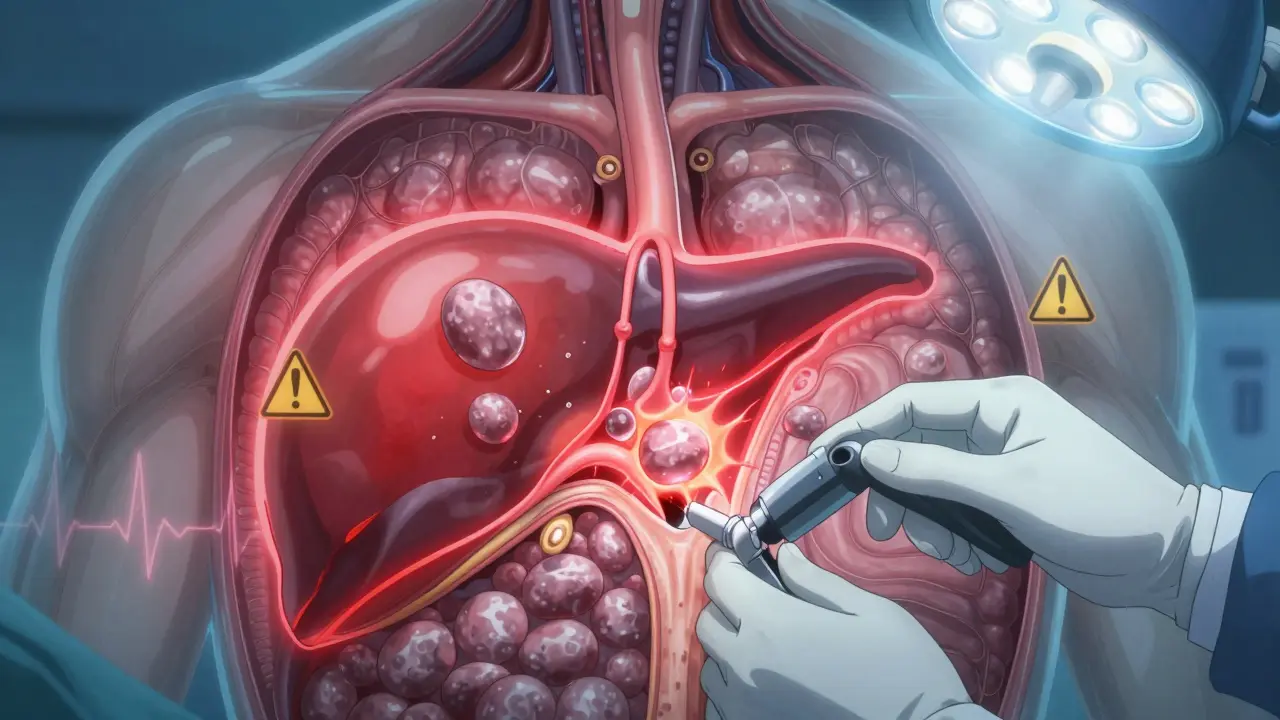
What Happens When Gallstones Block the Flow
Gallstones form when bile in the gallbladder gets out of balance. About 80% of them are made of cholesterol, the rest are pigment stones from bilirubin. They don’t cause pain unless they move and block the cystic duct-the tube that lets bile flow out of the gallbladder. When that happens, pressure builds up. The gallbladder contracts hard, trying to push bile through, and that’s what causes the pain.The pain usually starts suddenly, peaks within an hour, and lasts 1 to 5 hours. It’s centered in the upper right abdomen or just below the breastbone. It doesn’t come in waves like cramps. It’s constant. And it’s not helped by pooping, burping, or lying still. That’s how you know it’s not gas or indigestion.
Here’s the scary part: if the blockage lasts longer than a few hours, the gallbladder starts to swell and get infected. That’s acute cholecystitis. About 1 in 5 people with biliary colic will develop this. Symptoms get worse-fever, nausea, vomiting, and the pain becomes constant, even at rest. The skin might turn yellow if the stone slips into the common bile duct. That’s called jaundice. And if the stone blocks the pancreatic duct? That’s pancreatitis. All of these can land you in the ER.
Who Gets Gallstones-and Why
About 1 in 10 adults in Australia, the US, or Europe has gallstones. But 8 out of 10 never have symptoms. Only 1 to 3% of those silent stones turn painful each year. So why do some people suffer and others don’t?Women are 2 to 3 times more likely to get them than men. That’s because estrogen increases cholesterol in bile. Pregnancy, birth control pills, and hormone therapy all raise the risk. People over 40, especially those with obesity, are at higher risk too. The CDC says nearly 40% of US adults are obese-and that’s a major driver. Hispanic populations have a 45% higher rate than non-Hispanic whites. Rapid weight loss, diabetes, and a family history also play roles.
It’s not about diet alone. You can eat kale and still get gallstones. It’s about how your body processes bile. If your gallbladder doesn’t empty well, cholesterol crystallizes. If you’re overweight, your liver dumps more cholesterol into bile. Genetics matter too. If your mum had them, your risk goes up.
When to Consider Surgery
The first episode of biliary colic doesn’t always mean surgery. But here’s what the data says: more than 90% of people who’ve had one episode will have another within 10 years. Two-thirds will have a second one within just two years. And if you wait, 20 to 30% will end up in the hospital with complications like cholecystitis or pancreatitis within five years.That’s why doctors now recommend surgery for most people with symptoms. Not because it’s urgent right away-but because waiting increases your chances of a bad outcome. The American Academy of Family Physicians found that 64% of people who tried to avoid surgery ended up needing it within 5.6 years anyway.
There’s only one treatment that stops the problem for good: removing the gallbladder. That’s called a cholecystectomy. And today, 90% of these are done laparoscopically. That means four tiny cuts, a camera, and tools inserted through them. You’re usually home the next day. Recovery takes about a week, not a month. Open surgery? That’s rare now-only used when there’s severe infection, scarring, or anatomy too tricky to see.
Studies show 95% of patients are happy with the results. Pain disappears. No more midnight emergencies. No more avoiding pizza or fried chicken. One woman in Cleveland Clinic’s patient newsletter had 17 attacks over 18 months. After surgery, her pain was gone in 10 days. Back to work in two weeks.
What About Nonsurgical Options?
You might hear about pills or shock waves to dissolve stones. Ursodeoxycholic acid (UDCA) can dissolve small cholesterol stones-but only in 30 to 50% of cases. And it takes 6 to 24 months. Even then, half the people get the stones back within five years. Shock-wave lithotripsy breaks stones into pieces, but it’s rarely used now because the fragments often reblock ducts. It’s expensive, messy, and doesn’t fix the root problem: a gallbladder that’s already acting up.These methods are only considered for people who truly can’t have surgery-like someone with severe heart disease or who’s too frail. Even then, it’s a temporary fix. Surgery still wins every time.
When Surgery Isn’t the Best Choice
There’s an important exception: older adults with other health problems. A 75-year-old with heart disease, diabetes, and kidney issues has a much higher risk of dying from surgery than a healthy 45-year-old. A 2023 study showed 30-day mortality jumps from 0.1% in healthy patients to 2.8% in those with three or more conditions.For these patients, doctors may manage symptoms with diet changes, pain meds, and watchful waiting. Sometimes, they use a new technique-endoscopic ultrasound-guided gallbladder drainage. It’s not permanent, but it drains the infected gallbladder without removing it. It’s a bridge to better health, not a cure. Once the patient is stable, surgery might still be an option later.

What Happens After Surgery?
Most people feel better right away. But about 12% report ongoing diarrhea, especially after fatty meals. That’s because without the gallbladder, bile flows constantly into the intestine instead of being stored and released on demand. It’s not dangerous, but it can be annoying. Eating smaller, lower-fat meals helps. Most people adapt within a few months.A small group-about 6%-get what’s called post-cholecystectomy syndrome: persistent pain, bloating, or nausea. Sometimes it’s because another problem was missed-like a bile duct stone or irritable bowel. Sometimes, the pain was never from gallstones at all. That’s why getting the right diagnosis before surgery matters.
That’s also why so many patients report seeing three or more doctors before getting diagnosed. Gallstone pain mimics heartburn, pancreatitis, even a heart attack. Ultrasound is the gold standard test-quick, safe, and 95% accurate. If your doctor doesn’t order one after you describe classic biliary colic, ask why.
What to Expect Before and After
If you’re scheduled for surgery, you’ll be asked to fast for 6 to 8 hours before. No need for special diets beforehand. But if you’re overweight or diabetic, your surgeon might ask you to lose weight or get blood sugar under control first. That reduces risks.On the day of surgery, you’ll be under general anesthesia. The procedure takes 45 to 60 minutes. Most people wake up with mild shoulder pain-that’s from the gas used to inflate the belly during surgery. It goes away in a day.
Recovery is fast. You’ll be up and walking within 4 hours. Drink liquids within 6 hours. Most go home the next day. You can shower in 24 hours. Avoid heavy lifting for two weeks. Back to desk work? In a week. Back to the gym? In four.
Follow-up is minimal. No stitches to remove. Just a call from your surgeon’s office in two weeks to check in. If you develop fever, yellow skin, or severe pain after surgery, go back to the hospital. That’s rare, but it can mean a bile leak or infection.
The Bigger Picture
About 700,000 gallbladder removals are done each year in the US alone. The global market for gallstone treatments is growing-mostly because obesity and aging populations are rising. New techniques like single-incision laparoscopic surgery are being tried, but they come with higher complication rates. Standard laparoscopic surgery still wins.What’s changing is how we care for patients after surgery. Hospitals are adopting ERAS protocols-Enhanced Recovery After Surgery. That means getting patients moving fast, eating early, and minimizing pain meds. The result? 30% shorter hospital stays and 25% fewer readmissions.
Experts agree: for most people with symptomatic gallstones, cholecystectomy is the best choice. It’s safe, effective, and life-changing. Waiting doesn’t make it go away. It just makes the next attack worse.
If you’ve had even one episode of that classic right-sided pain-especially after eating-you should talk to your doctor. Don’t wait for the next attack. Don’t assume it’s just a bad meal. Get an ultrasound. Know your options. And if surgery is recommended, understand that it’s not just removing a stone-it’s removing the risk of something far worse.





It’s wild how something so common can be so misunderstood. I had no idea gallstones could mimic a heart attack until my aunt ended up in the ER thinking she was having one. Turns out, it was just her gallbladder screaming. The article nailed it-this isn’t indigestion. It’s a warning. And honestly, most people just pop an antacid and hope it goes away. We need way more public awareness about this.